|
| | مكتبة الصور الطبية : - باثولوجى -- Pathology slides |  |
| | | كاتب الموضوع | رسالة |
|---|
ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الأحد 18 نوفمبر 2018, 11:57 pm الأحد 18 نوفمبر 2018, 11:57 pm | |
| |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الأحد 18 نوفمبر 2018, 11:59 pm الأحد 18 نوفمبر 2018, 11:59 pm | |
| Patholgy Slides : Cell Injury and Adaptation اضغط على الصورة للتكبير - Click on image to enlarge size Fatty change liver steatosis Fatty change or Steatosis represents the intracytoplasmic accumulation of triglyceride (neutral fats) of parenchimal organs, such as: liver, myocardium and kidney. Mechanisms : increase of free fatty acids (starvation, diabetes and chronic ethylism/alcoholism), reduction of free fatty acids oxidation (hypoxia, toxins, chronic ethylism/alcoholism), increase of esterification of free fatty acids into triglycerides (due to increased free fatty acids or reduction of their oxidation, chronic ethylism/alcoholism) and reduced export of tryglicerides due to deficiency of lipid binding apoprotein (starvation/malnutrition, toxins). Initially, fatty change does not impair the cells function, being reversible. At the beginning, the hepatocytes present small fat vacuoles in the vicinity of the endoplasmic reticulum (liposomes) - microvesicular fatty change (photo). In the late stages, the size of the vacuoles increases pushing the nucleus to the periphery of the cell - macrovesicular fatty change. These vesicles are well delineated and optically "empty" because fat solves during tissue processing (paraffin embedding). Large vacuoles may coalesce, producing fatty cysts - which are irreversible lesions. (HE, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Cholesterolosis of the gallbladder Cholesterolosis of the gallbladder. (HE, ob x4) Cholesterolosis of the gallbladder (detail of an enlarged mucosal fold). (HE, ob x10)
Cholesterolosis is an intracellular accumulation of lipids (cholesterol). When cholesterol is in
excess in the bile, it passes into the lamina propria where is phagocitated by macrophages. These macrophages become larger and polygonal, with foamy cytoplasm and small, hyperchromatic, central nucleus (xantic cells). Aggregation of xantic cells may enlarge the mucosal folds, producing a polypoid appearance of the mucosal surface. At gross examination, these yellow micropolyps (1-2 mm) contrasts with the red aspect of the surrounding mucosa, hence the term "strawberry gallbladder".
Sometimes, cholesterolosis is associated with inflammation of the gallbladder (cholecystitis) or with gallstones (cholelithiasis) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Amyloidosis (kidney) Amyloid (an abnormal protein) accumulates as extra-cellular deposits, nodular or diffuse, as pink, amorphous material. Initially, the deposits appear in the glomeruli: within the mesangial matrix and along the basement membranes of the capillary loops. Continuous accumulation of the amyloid will compress and obliterate the capillary tuft. With progression, amyloid deposits appear also peritubular and within the arteriolar wall, narrowing them. Congo red is a special staining, elective for amyloid. (Congo Red, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Hyaline arteriolosclerosis (Benign nephrosclerosis) In benign hypertension, hyaline (pink, amorphous, homogeneous material) accumulates in the wall of small arteries and arterioles, producing the thickening of their walls and the narrowing of the lumens. Consequent ischemia will produce tubular atrophy, interstitial fibrosis, glomerular alterations (smaller glomeruli with different degrees of hyalinization - from mild to sclerosis of glomeruli) and periglomerular fibrosis. (Hematoxylin-eosine, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Cellular swelling (liver) Cellular swelling (synonyms : hydropic change, vacuolar degeneration, cellular edema) is an acute reversible change resulting as a response to nonlethal injuries. It is an intracytoplasmic accumulation of water due to incapacity of the cells to maintain the ionic and fluid homeostasis. It is easy to be observed in parenchymal organs : liver (hepatitis, hypoxia), kidney (shock), myocardium (hypoxia, phosphates intoxication). It may be local or diffuse, affecting the whole organ. ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
atlas of pathology
|
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الأحد 18 نوفمبر 2018, 11:59 pm الأحد 18 نوفمبر 2018, 11:59 pm | |
| Patholgy Slides : Acute inflammation اضغط على الصورة للتكبير - Click on image to enlarge size Acute inflammation (exudative inflammation) is the immediate and early defensive response in the host, to all forms of injury. The main characteristic feature is the inflammatory infiltrate (exudate), which consists in: plasma liquid, plasma proteins, leukocytes, red blood cells and, sometimes, infective germs. Depending on the etiology, localization and composition, exudative inflammation can be : serous (first stage of lobar pneumonia, vesicles in herpetic infections or burns) fibrinous (second stage of lobar pneumonia, fibrinous pericarditis, peritonitis or pleuresia, pseudomembranous colitis) sero-fibrinous (the mixed form of previous two) chataral (inflammation of mucus secreting mucosa from digestive or respiratory tract) purulent or suppurative (localized - abscess and folliculitis or diffuse - phlegmon or cellulitis, erysipelas, purulent meningitis, phlegmonous cholecistitis/appendicitis) ............................................................... Fibrinous pericarditis Fibrinous pericarditis is an exudative inflammation. The visceral pericardium (epicardium) is infiltrated by the fibrinous exudate. This consists in fibrin strands and leukocytes. Fibrin describes an eosinophilic (pink) network, amorphous. Leukocytes (mainly, neutrophils) are found within the fibrin deposits and intrapericardic. Vascular congestion is also present. The myocardium has no changes. (Hematoxylin-eosine, ob. x4)  Fibrinous pericarditis (Hematoxylin-eosine, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــPurulent meningitis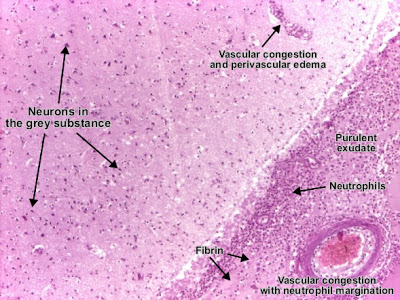 Purulent leptomeningitis (suppurative leptomeningitis) is a diffuse purulent inflammation. The leptomeninges (arachnoida and piamater) contain purulent exudate (pus): leukocytes (neutrophils), fibrin, germs, proteins, necrotic debris. Blood vessels in the subarachnoidian space and those intracerebral are congested and neutrophil margination is present. (Hematoxylin-eosine, ob. x4)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAbscess brain Purulent leptomeningitis (suppurative leptomeningitis) is a diffuse purulent inflammation. The leptomeninges (arachnoida and piamater) contain purulent exudate (pus): leukocytes (neutrophils), fibrin, germs, proteins, necrotic debris. Blood vessels in the subarachnoidian space and those intracerebral are congested and neutrophil margination is present. (Hematoxylin-eosine, ob. x4)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAbscess brain Abscess is an exudative purulent localized inflammation. In the white matter, a recent abscess consisting in pus : neutrophils (normal or in lisis), fibrin, necrotic debris, germs. Vessels present congestion and important perivascular edema. (Hematoxylin-eosine, ob. x4)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAcute pyelonephritis Abscess is an exudative purulent localized inflammation. In the white matter, a recent abscess consisting in pus : neutrophils (normal or in lisis), fibrin, necrotic debris, germs. Vessels present congestion and important perivascular edema. (Hematoxylin-eosine, ob. x4)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAcute pyelonephritis Acute pyelonephritis is an exudative purulent localized inflammation of kidney and renal pelvis. The renal parenchyma presents in the interstitium abscesses (suppurative necrosis), consisting in purulent exudate (pus): neutrophils, fibrin, cell debris and central germ colonies (hematoxylinophils). Tubules are damaged by exudate and may contain neutrophil casts. In the early stages, glomeruli and vessels are normal. (Hematoxylin-eosine, ob. x10) Acute pyelonephritis is an exudative purulent localized inflammation of kidney and renal pelvis. The renal parenchyma presents in the interstitium abscesses (suppurative necrosis), consisting in purulent exudate (pus): neutrophils, fibrin, cell debris and central germ colonies (hematoxylinophils). Tubules are damaged by exudate and may contain neutrophil casts. In the early stages, glomeruli and vessels are normal. (Hematoxylin-eosine, ob. x10) Acute pyelonephritis (Hematoxylin-eosine, ob. x10) Acute pyelonephritis (Hematoxylin-eosine, ob. x10) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:00 am الإثنين 19 نوفمبر 2018, 12:00 am | |
| Patholgy Slides : Chronic inflammation اضغط على الصورة للتكبير - Click on image to enlarge size Chronic inflammation is a long lasting inflammation (weeks or months) due to persistent aggressive stimuli and is characterized by: active inflammation with mononuclear cells, tissue destruction and repair. It can follow acute inflammation or can be chronic right from the beginning. Types of chronic inflammation : unspecific (e.g. : chronic peptic ulcer) and specific (granulomatous). According to the mechanism, granulomatous inflammation may be: immune type (tuberculosis, sarcoidosis) and non-immune type (foreign body reaction). Classification of granulomatous inflammation, according to the etiology : [list=roman_mare] [*] Infectious granuloma :
- Bacterial :
- Mycobacterium tuberculosis (Koch bacillus) - Tuberculosis
- Mycobacterium leprae - Leprosy
- Treponema pallidum - Syphilis
- Gram-positive bacillus (Actinomyces israeli) - Actinomycosis
- Gram-negative bacillus (Bartonella henselae) - Cat-scratch disease
Parasitic :
Toxoplasma gondii - Toxoplasmosis
Helminths - Cysticercosis
Fungi (Candida albicans) - Candidiasis
[*] Foreign body granuloma[*] Unknown etiology granuloma :
- Sarcoidosis
- Crohn's disease
[/list]
Tuberculous lymphadenitis : tuberculous granuloma
Tuberculous lymphadenitis is a chronic specific granulomatous inflammation with caseation necrosis. The characteristic morphological element is the tuberculous granuloma (caseating tubercule) : giant multinucleated cells (Langhans cells), surrounded by epithelioid cells aggregates, T cell lymphocytes and few fibroblasts. Granulomatous tubercules evolve to central caseous necrosis and tend to become confluent, replacing the lymphoid tissue. (H&E, ob. x4)  Tuberculous granuloma. Multinucleated giant cell (mature - Langhans type) : 50 - 100 microns, numerous small nuclei (over 20) disposed at the periphery of the cell (crown or horseshoe), abundant eosinophilic cytoplasm. It results when activated macrophages merge. Epithelioid cells are activated macrophages resembling epithelial cells : elongated, with finely granular, pale eosinophilic (pink) cytoplasm and central, ovoid nucleus. They have indistinct shape contour and form aggregates. At the periphery are the lymphocytes (T cells) and rare plasma cells and fibroblasts. Caseous necrosis is a central area, amorphous, finely granular, eosinophilic (pink). If recent, it may contain nuclear fragments. The caseum is the result of giant cells and epithelioid cells destruction. (Hematoxylin-eosin, ob. x20) Tuberculous granuloma (Hematoxylin-eosin, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Pulmonary tuberculosis Tuberculosis is a chronic inflammation caused by Mycobacterium tuberculosis (tubercle bacillus, Koch bacillus) - human type or bovine type. The most affected organ by tuberculosis is the lung. Microscopically, the characteristic lesion in tuberculosis is the tuberculous granuloma. Pulmonary tuberculosis. Tuberculous granuloma is localized in the pulmonary interstitium, compressing the surrounding alveoli and destroing the parenchyma. (Hematoxylin-eosin, ob. x4) (For detailed histological description of granuloma Tuberculous granuloma in the pulmonary interstitium. (Hematoxylin-eosin, ob. X20) Tuberculous granuloma in the pulmonary interstitium. (Hematoxylin-eosin, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Foreign body granuloma Foreign body granuloma has a non-immune mechanism. Foreign body granuloma is a reaction to exogenous materials (talc, suture material, parasites, oil droplets, wood, metals, silica, silicon) or endogenous (hail shafts, keratin, cholesterol, urates/goutous tophi), which are immunologically inert. Microscopically, foreign body granuloma to suture material (nylon, silk) contains multinucleated giant cells, with haphazardly arranged nuclei. These giant cells are fused macrophages. The foreign body is birefringent, and sometimes may be visible by polarized light in the middle of the granuloma or inside the giant cells. These granulomas are non-necrotic. (HE, ob. x4) Foreign body granuloma (suture material) (HE, ob. x10). |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:01 am الإثنين 19 نوفمبر 2018, 12:01 am | |
| Patholgy Slides : Regeneration and Repair by Connective Tissue اضغط على الصورة للتكبير - Click on image to enlarge size
After destruction, cells and tissues can be replaced by vital cells through parenchymal regeneration or by connective tissue repair.
Repair by connective tissue starts with formation of granulation tissue. It may appear in chronic peptic ulcer, surrounding necrotic areas (infarct, inflammation) or fibrin (fibrinous inflammation, thrombus). With time, the maturation of granulation tissue will replace the damaged area with a scar
Granulation tissue

Healing (repair) by connective tissue has the granulation tissue as a hallmark. It consists of new capillaries (result of proliferation of endothelial cells - angiogenesis or neovascularization) in an edematous atmosphere of fibroblasts (spindle shaped), myofibroblasts, mononuclear inflammatory cells, macrophages, neutrophils, cellular debris. (Hematoxylin-eosin, ob. x10)
ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Organization of a venous thrombus

Pulmonary vein completely obliterated by a thrombus with organization. The thrombus was replaced by an immature granulation tissue, rich in newly formed capillaries, fibroblasts, collagen and reduced inflammatory infiltrate. (Hematoxylin-eosin, ob. x4)Patholgy Slides : Tumors or Neoplasia
Benign epithelial tumors
اضغط على الصورة للتكبير - Click on image to enlarge size
Squamous cell papilloma (skin)

[size=13]Squamous cell papilloma (verruca vulgaris) is a benign epithelial tumor. Tumor cells proliferate and produce finger-like or warty projections; secondary, the subjacent vessels and connective tissue (fibrovascular core) grows to sustain and feed the tumor. The tumor cells resemble normal squamous cells, but there is an increase of the layers number: acanthosis, hypergranulosis and hyperkeratosis. The basement membrane is intact. (H&E, ob. X10)
ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAdenomatous tubulo-villous polyp, pedunculated (colon)Adenoma is a benign epithelial tumor arising in epithelium of mucosa (stomach, small intestine and bowel), glands (endocrine and exocrine) and ducts. In hollow organs (e.g. digestive tract) the adenoma grows upwards into the lumen - adenomatous polyp or polypoid adenoma. Depending on the type of the insertion base, adenoma may be pedunculated (lobular head with a long, slender stalk, covered by normal mucosa - see photo) or sessile (broad base). If not elevated above the surface of the mucosa, the adenoma is called flat adenoma Adenomatous tubulo-villous polyp, pedunculated (colon). The adenomatous proliferation is characterized by different degrees of cell dysplasia (cellular and architectural atypia) : loss of normal differentiation of epithelium, irregular cells with hyperchromatic nuclei, (pseudo)stratified nuclei, nucleolus, decreased mucosecretion and mitosis. The architecture may be tubular, villous or tubulo-villous. Basement membrane and muscularis mucosae are intact. (HE, ob. x4)Detail of an adenomatous tubulo-villous polyp (colon) Adenomatous tubulo-villous polyp, pedunculated (colon). The adenomatous proliferation is characterized by different degrees of cell dysplasia (cellular and architectural atypia) : loss of normal differentiation of epithelium, irregular cells with hyperchromatic nuclei, (pseudo)stratified nuclei, nucleolus, decreased mucosecretion and mitosis. The architecture may be tubular, villous or tubulo-villous. Basement membrane and muscularis mucosae are intact. (HE, ob. x4)Detail of an adenomatous tubulo-villous polyp (colon)  Compared to normal colonic epithelium (lower left corner of the picture) the adenomatous proliferation is characterized by different degrees of cell dysplasia and tubular, villous or tubulo-villousarchitecture. In tubular component tumor cells proliferate generating tubular shapes, more or less irregular or branched. The villous pattern presents villi - finger-like projections lined by dysplastic epithelium and with thin fibro-vascular core. Passage from tumoral epithelium to normal mucosa is abrupt. (HE, ob. x10)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAdenomatous villous polyp, sessile (colon)Adenoma is a benign epithelial tumor arising in epithelium of mucosa (stomach, small intestine and bowel), glands (endocrine and exocrine) and ducts. Compared to normal colonic epithelium (lower left corner of the picture) the adenomatous proliferation is characterized by different degrees of cell dysplasia and tubular, villous or tubulo-villousarchitecture. In tubular component tumor cells proliferate generating tubular shapes, more or less irregular or branched. The villous pattern presents villi - finger-like projections lined by dysplastic epithelium and with thin fibro-vascular core. Passage from tumoral epithelium to normal mucosa is abrupt. (HE, ob. x10)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــAdenomatous villous polyp, sessile (colon)Adenoma is a benign epithelial tumor arising in epithelium of mucosa (stomach, small intestine and bowel), glands (endocrine and exocrine) and ducts.
In hollow organs (e.g. digestive tract) the adenoma grows upwards into the lumen - adenomatous polyp or polypoid adenoma. Depending on the type of the insertion base, adenoma may be pedunculated (lobular head with a long, slender stalk, covered by normal mucosa) or sessile (broad base - see photo). If not elevated above the surface of the mucosa, the adenoma is called flat adenoma Adenomatous villous polyp, sessile (colon). The adenomatous proliferation is characterized by different degrees of cell dysplasia (cellular and architectural atypia): loss of normal differentiation of epithelium, irregular cells with hyperchromatic nuclei, (pseudo)stratified nuclei, nucleolus, decreased mucosecretion and atypical mitosis. The architecture may be tubular, villous (photo) or tubulo-villous. Basement membrane and muscularis mucosae are intact. (HE, ob. x4)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــFibroadenoma of the breast Adenomatous villous polyp, sessile (colon). The adenomatous proliferation is characterized by different degrees of cell dysplasia (cellular and architectural atypia): loss of normal differentiation of epithelium, irregular cells with hyperchromatic nuclei, (pseudo)stratified nuclei, nucleolus, decreased mucosecretion and atypical mitosis. The architecture may be tubular, villous (photo) or tubulo-villous. Basement membrane and muscularis mucosae are intact. (HE, ob. x4)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــFibroadenoma of the breast  Fibroadenoma of the breast is a benign tumor composed of two elements : epithelium and stroma. It is nodular and encapsulated, included in breast. The epithelial proliferation appears in a single terminal ductal unit and describes duct-like spaces surrounded by a fibroblastic stroma. Depending on the proportion and the relationship between these two components, there are two main histological features : intracanalicular and pericanalicular. Often, both types are found in the same tumor. Intracanalicular fibroadenoma (photo A) : stromal proliferation predominates and compresses the ducts, which are irregular, reduced to slits. Pericanalicular fibroadenoma (photo B) : fibrous stroma proliferates around the ductal spaces, so that they remain round or oval, on cross section. The basement membrane is intact. (H&E, ob. x10)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Fibroadenoma of the breast is a benign tumor composed of two elements : epithelium and stroma. It is nodular and encapsulated, included in breast. The epithelial proliferation appears in a single terminal ductal unit and describes duct-like spaces surrounded by a fibroblastic stroma. Depending on the proportion and the relationship between these two components, there are two main histological features : intracanalicular and pericanalicular. Often, both types are found in the same tumor. Intracanalicular fibroadenoma (photo A) : stromal proliferation predominates and compresses the ducts, which are irregular, reduced to slits. Pericanalicular fibroadenoma (photo B) : fibrous stroma proliferates around the ductal spaces, so that they remain round or oval, on cross section. The basement membrane is intact. (H&E, ob. x10)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ[/size] |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:03 am الإثنين 19 نوفمبر 2018, 12:03 am | |
| Patholgy Slides : Tumors or Neoplasia Malignant epithelial tumorsاضغط على الصورة للتكبير - Click on image to enlarge sizeSquamous cell carcinoma (skin) Squamous cell carcinoma is a malignant epithelial tumor which originates in epidermis, squamous mucosa or areas of squamous metaplasia. In skin, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis). In well differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus). Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses. Tumor cells transform into keratinized squames and form round nodules with concentric, laminated layers, called "cell nests"or "epithelial/keratinous pearls". The surrounding stroma is reduced and contains inflammatory infiltrate (lymphocytes). Poorly differentiated squamous carcinomas contain more pleomorphic cells and no keratinization. (H&E, ob. x10) Squamous cell carcinoma is a malignant epithelial tumor which originates in epidermis, squamous mucosa or areas of squamous metaplasia. In skin, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis). In well differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus). Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses. Tumor cells transform into keratinized squames and form round nodules with concentric, laminated layers, called "cell nests"or "epithelial/keratinous pearls". The surrounding stroma is reduced and contains inflammatory infiltrate (lymphocytes). Poorly differentiated squamous carcinomas contain more pleomorphic cells and no keratinization. (H&E, ob. x10) Squamous cell carcinoma (skin). Tumor cells transformed into keratinized squames form round nodules with concentric, laminated layers, called "cell nests" or "epithelial/keratinous pearls". (H&E, ob. X40)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــBasal cell carcinoma Squamous cell carcinoma (skin). Tumor cells transformed into keratinized squames form round nodules with concentric, laminated layers, called "cell nests" or "epithelial/keratinous pearls". (H&E, ob. X40)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــBasal cell carcinoma Basal cell carcinoma is a malignant epithelial tumor arising only in skin, from the basal layer of the epidermis or of the pilosebaceous adnexa. Tumor is represented by compact areas, well delineated and invading the dermis, apparent with no connection with the epidermis. Tumor cells resemble normal basal cells (small, monomorphous) are disposed in palisade at the periphery of the tumor nests, but are spindle-shaped and irregular in the middle. Tumor clusters are separated by a reduced stroma with inflammatory infiltrate. (H&E, ob. x4) Basal cell carcinoma is a malignant epithelial tumor arising only in skin, from the basal layer of the epidermis or of the pilosebaceous adnexa. Tumor is represented by compact areas, well delineated and invading the dermis, apparent with no connection with the epidermis. Tumor cells resemble normal basal cells (small, monomorphous) are disposed in palisade at the periphery of the tumor nests, but are spindle-shaped and irregular in the middle. Tumor clusters are separated by a reduced stroma with inflammatory infiltrate. (H&E, ob. x4)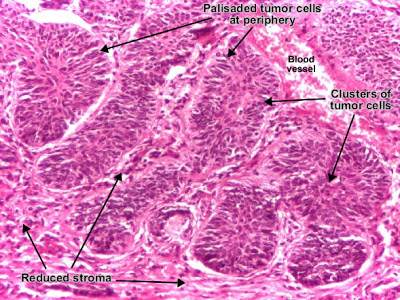 Basal cell carcinoma (detailBasal cell carcinoma. (H&E, ob. X40)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــGastric carcinoma, intestinal typeGastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Basal cell carcinoma (detailBasal cell carcinoma. (H&E, ob. X40)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــGastric carcinoma, intestinal typeGastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, intestinal type. Tumor cells describe irregular tubular structures, with stratification, multiple lumens surrounded by a reduced stroma ("back to back" aspect). The tumor invades the gastric wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Often it associates intestinal metaplasia in adjacent mucosa. Depending on glandular architecture, cellular pleomorphism and mucosecretion, adenocarcinoma may present 3 degrees of differentiation : well (photo), moderate and poorly differentiate. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type. Tumor cells describe irregular tubular structures, with stratification, multiple lumens surrounded by a reduced stroma ("back to back" aspect). The tumor invades the gastric wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Often it associates intestinal metaplasia in adjacent mucosa. Depending on glandular architecture, cellular pleomorphism and mucosecretion, adenocarcinoma may present 3 degrees of differentiation : well (photo), moderate and poorly differentiate. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type, infiltrating muscularis propria. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type, infiltrating muscularis propria. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type. (H&E, ob. X40)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــGastric carcinoma, diffuse type (mucinous)Gastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, intestinal type. (H&E, ob. X40)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــGastric carcinoma, diffuse type (mucinous)Gastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, diffuse (infiltrative) type. Tumor cells are discohesive and secrete mucus which is delivered in the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated (Lauren classification). If the mucus remains inside the tumor cell, it pushes the nucleus against the cell membrane - "signet-ring cell". (H&E, ob. x10) Gastric adenocarcinoma, diffuse (infiltrative) type. Tumor cells are discohesive and secrete mucus which is delivered in the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated (Lauren classification). If the mucus remains inside the tumor cell, it pushes the nucleus against the cell membrane - "signet-ring cell". (H&E, ob. x10) Gastric adenocarcinoma, diffuse type. (H&E, ob. X20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــModerately differentiated adenocarcinoma (colon) Gastric adenocarcinoma, diffuse type. (H&E, ob. X20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــModerately differentiated adenocarcinoma (colon)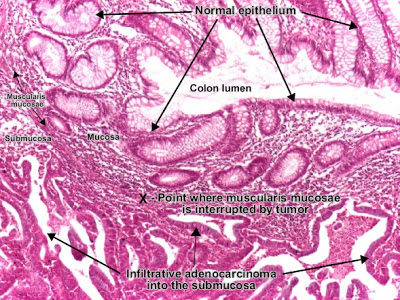 Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa (photo) and thence the muscularis propria. (Notice the end-point of muscularis mucosae. At left from this point, muscularis mucosae is continuous. At right from this point, muscularis mucosae is destroyed by tumor cells invasion.) Tumor cells describe irregular tubular structures, harboring stratification, multiple lumens, reduced stroma ("back to back" aspect). Depending on glandular architecture, cellular pleomorphism and mucosecretion of the predominant pattern, adenocarcinoma may present 3 degrees of differentiation: well, moderate and poorly differentiate. (H&E, ob. x10)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــPoorly differentiated adenocarcinoma (mucinous), colon Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa (photo) and thence the muscularis propria. (Notice the end-point of muscularis mucosae. At left from this point, muscularis mucosae is continuous. At right from this point, muscularis mucosae is destroyed by tumor cells invasion.) Tumor cells describe irregular tubular structures, harboring stratification, multiple lumens, reduced stroma ("back to back" aspect). Depending on glandular architecture, cellular pleomorphism and mucosecretion of the predominant pattern, adenocarcinoma may present 3 degrees of differentiation: well, moderate and poorly differentiate. (H&E, ob. x10)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــPoorly differentiated adenocarcinoma (mucinous), colon Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Tumor cells are discohesive and secrete mucus which invades the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated. If the mucus remains inside the tumor cell, it pushes the nucleus at the periphery, against the cell membrane - "signet-ring cell". (H&E, ob. x20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــPoorly differentiated hepatocellular carcinoma Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Tumor cells are discohesive and secrete mucus which invades the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated. If the mucus remains inside the tumor cell, it pushes the nucleus at the periphery, against the cell membrane - "signet-ring cell". (H&E, ob. x20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــPoorly differentiated hepatocellular carcinoma Hepatocellular carcinoma, poorly differentiated (photo - upper right), developed on liver cirrhosis. This malignant epithelial tumor consists in tumor cells, discohesive, pleomorphic, anaplastic, giant. The tumor has a scant stroma and central necrosis because of the poor vascularization. In well differentiated forms, tumor cells resemble hepatocytes, form cords and nests, and may contain bile pigment in cytoplasm. (H&E, ob. x20) Hepatocellular carcinoma, poorly differentiated (photo - upper right), developed on liver cirrhosis. This malignant epithelial tumor consists in tumor cells, discohesive, pleomorphic, anaplastic, giant. The tumor has a scant stroma and central necrosis because of the poor vascularization. In well differentiated forms, tumor cells resemble hepatocytes, form cords and nests, and may contain bile pigment in cytoplasm. (H&E, ob. x20) Poorly differentiated hepatocellular carcinoma. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــRenal cell carcinoma (Grawitz tumor) Poorly differentiated hepatocellular carcinoma. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــRenal cell carcinoma (Grawitz tumor)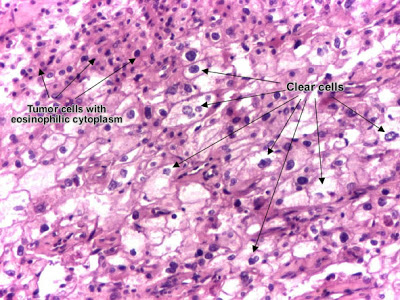 Renal clear cell carcinoma (Grawitz tumor) is a malignant epithelial tumor resulted from proliferation of tubule cells. Tumor cells form cords, papillae, tubules or nests, and are atypical, polygonal and large. Because these cells accumulate glycogen and lipids, their cytoplasm appears "clear", lipid-laden, the nuclei remain in the middle of the cells, and the cellular membrane is evident. Some cells may be smaller, with eosinophilic cytoplasm, resembling normal tubular cells. The stroma is reduced, but well vascularized. The tumor grows in large front, compressing the surrounding parenchyma, producing a pseudocapsule. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــEndometrioid carcinoma of endometrium Renal clear cell carcinoma (Grawitz tumor) is a malignant epithelial tumor resulted from proliferation of tubule cells. Tumor cells form cords, papillae, tubules or nests, and are atypical, polygonal and large. Because these cells accumulate glycogen and lipids, their cytoplasm appears "clear", lipid-laden, the nuclei remain in the middle of the cells, and the cellular membrane is evident. Some cells may be smaller, with eosinophilic cytoplasm, resembling normal tubular cells. The stroma is reduced, but well vascularized. The tumor grows in large front, compressing the surrounding parenchyma, producing a pseudocapsule. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــEndometrioid carcinoma of endometrium Endometrioid adenocarcinoma of the endometrium is a malignant epithelial tumor. It appears on a background of endometrial hyperplasia, in hyperestrogenism. Tumor cells are atypical and form irregular glands, with multiple lumens, stratification. The stroma is reduced, producing the "back to back" aspect of the tumor glands. The myometrium is not infiltrated. (H&E, ob. x10) Endometrioid adenocarcinoma of the endometrium is a malignant epithelial tumor. It appears on a background of endometrial hyperplasia, in hyperestrogenism. Tumor cells are atypical and form irregular glands, with multiple lumens, stratification. The stroma is reduced, producing the "back to back" aspect of the tumor glands. The myometrium is not infiltrated. (H&E, ob. x10) Endometrioid adenocarcinoma of the endometrium. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــInvasive ductal carcinoma of the breast Endometrioid adenocarcinoma of the endometrium. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــInvasive ductal carcinoma of the breast Invasive (infiltrating) ductal carcinoma of the breast is a malignant epithelial tumor resulted from proliferation of ductal epithelium of breast. It is the most common type of breast cancer (70 - 80 %). Atypical tumor cells form ribbons, tubules or nests, broke the basement membrane of the duct and infiltrate the surrounding tissues (fat tissue - photo, skeletal muscle and/or skin). Tumor cells induce desmoplastic reaction in stroma (abundant fibrosis, collagen). (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــCarcinoma metastasis (lymph node) Invasive (infiltrating) ductal carcinoma of the breast is a malignant epithelial tumor resulted from proliferation of ductal epithelium of breast. It is the most common type of breast cancer (70 - 80 %). Atypical tumor cells form ribbons, tubules or nests, broke the basement membrane of the duct and infiltrate the surrounding tissues (fat tissue - photo, skeletal muscle and/or skin). Tumor cells induce desmoplastic reaction in stroma (abundant fibrosis, collagen). (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــCarcinoma metastasis (lymph node) Lymph node with carcinoma metastasis : clusters of tumor cells, atypical, with carcinomatous character. (H&E, ob. x20) Lymph node with carcinoma metastasis : clusters of tumor cells, atypical, with carcinomatous character. (H&E, ob. x20) Detail from metastatic lymphadenopathy. (H&E, ob. x40) Detail from metastatic lymphadenopathy. (H&E, ob. x40) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:04 am الإثنين 19 نوفمبر 2018, 12:04 am | |
| Patholgy Slides : Tumors or Neoplasia Malignant epithelial tumors اضغط على الصورة للتكبير -ـ Click on image to enlarge size Squamous cell carcinoma (skin)  Squamous cell carcinoma is a malignant epithelial tumor which originates in epidermis, squamous mucosa or areas of squamous metaplasia. In skin, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis). In well differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus). Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses. Tumor cells transform into keratinized squames and form round nodules with concentric, laminated layers, called "cell nests"or "epithelial/keratinous pearls". The surrounding stroma is reduced and contains inflammatory infiltrate (lymphocytes). Poorly differentiated squamous carcinomas contain more pleomorphic cells and no keratinization. (H&E, ob. x10)  Squamous cell carcinoma (skin). Tumor cells transformed into keratinized squames form round nodules with concentric, laminated layers, called "cell nests" or "epithelial/keratinous pearls". (H&E, ob. X40) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Basal cell carcinoma Basal cell carcinoma is a malignant epithelial tumor arising only in skin, from the basal layer of the epidermis or of the pilosebaceous adnexa. Tumor is represented by compact areas, well delineated and invading the dermis, apparent with no connection with the epidermis. Tumor cells resemble normal basal cells (small, monomorphous) are disposed in palisade at the periphery of the tumor nests, but are spindle-shaped and irregular in the middle. Tumor clusters are separated by a reduced stroma with inflammatory infiltrate. (H&E, ob. x4) Basal cell carcinoma (detail Basal cell carcinoma. (H&E, ob. X40) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Gastric carcinoma, intestinal type Gastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, intestinal type. Tumor cells describe irregular tubular structures, with stratification, multiple lumens surrounded by a reduced stroma ("back to back" aspect). The tumor invades the gastric wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Often it associates intestinal metaplasia in adjacent mucosa. Depending on glandular architecture, cellular pleomorphism and mucosecretion, adenocarcinoma may present 3 degrees of differentiation : well (photo), moderate and poorly differentiate. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type, infiltrating muscularis propria. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type. (H&E, ob. X40) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Gastric carcinoma, diffuse type (mucinous) Gastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, diffuse (infiltrative) type. Tumor cells are discohesive and secrete mucus which is delivered in the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated (Lauren classification). If the mucus remains inside the tumor cell, it pushes the nucleus against the cell membrane - "signet-ring cell". (H&E, ob. x10) Gastric adenocarcinoma, diffuse type. (H&E, ob. X20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Moderately differentiated adenocarcinoma (colon) Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa (photo) and thence the muscularis propria. (Notice the end-point of muscularis mucosae. At left from this point, muscularis mucosae is continuous. At right from this point, muscularis mucosae is destroyed by tumor cells invasion.) Tumor cells describe irregular tubular structures, harboring stratification, multiple lumens, reduced stroma ("back to back" aspect). Depending on glandular architecture, cellular pleomorphism and mucosecretion of the predominant pattern, adenocarcinoma may present 3 degrees of differentiation: well, moderate and poorly differentiate. (H&E, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Poorly differentiated adenocarcinoma (mucinous), colon Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Tumor cells are discohesive and secrete mucus which invades the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated. If the mucus remains inside the tumor cell, it pushes the nucleus at the periphery, against the cell membrane - "signet-ring cell". (H&E, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Poorly differentiated hepatocellular carcinoma Hepatocellular carcinoma, poorly differentiated (photo - upper right), developed on liver cirrhosis. This malignant epithelial tumor consists in tumor cells, discohesive, pleomorphic, anaplastic, giant. The tumor has a scant stroma and central necrosis because of the poor vascularization. In well differentiated forms, tumor cells resemble hepatocytes, form cords and nests, and may contain bile pigment in cytoplasm. (H&E, ob. x20) Poorly differentiated hepatocellular carcinoma. (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Renal cell carcinoma (Grawitz tumor) Renal clear cell carcinoma (Grawitz tumor) is a malignant epithelial tumor resulted from proliferation of tubule cells. Tumor cells form cords, papillae, tubules or nests, and are atypical, polygonal and large. Because these cells accumulate glycogen and lipids, their cytoplasm appears "clear", lipid-laden, the nuclei remain in the middle of the cells, and the cellular membrane is evident. Some cells may be smaller, with eosinophilic cytoplasm, resembling normal tubular cells. The stroma is reduced, but well vascularized. The tumor grows in large front, compressing the surrounding parenchyma, producing a pseudocapsule. (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Endometrioid carcinoma of endometrium Endometrioid adenocarcinoma of the endometrium is a malignant epithelial tumor. It appears on a background of endometrial hyperplasia, in hyperestrogenism. Tumor cells are atypical and form irregular glands, with multiple lumens, stratification. The stroma is reduced, producing the "back to back" aspect of the tumor glands. The myometrium is not infiltrated. (H&E, ob. x10) Endometrioid adenocarcinoma of the endometrium. (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Invasive ductal carcinoma of the breast Invasive (infiltrating) ductal carcinoma of the breast is a malignant epithelial tumor resulted from proliferation of ductal epithelium of breast. It is the most common type of breast cancer (70 - 80 %). Atypical tumor cells form ribbons, tubules or nests, broke the basement membrane of the duct and infiltrate the surrounding tissues (fat tissue - photo, skeletal muscle and/or skin). Tumor cells induce desmoplastic reaction in stroma (abundant fibrosis, collagen). (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Carcinoma metastasis (lymph node) Lymph node with carcinoma metastasis : clusters of tumor cells, atypical, with carcinomatous character. (H&E, ob. x20) Detail from metastatic lymphadenopathy. (H&E, ob. x40) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:06 am الإثنين 19 نوفمبر 2018, 12:06 am | |
| Patholgy Slides : Tumors or Neoplasia Benign connective tissue tumors اضغط على الصورة للتكبير -ـ Click on image to enlarge sizeBenign tumors of the connective tissue gather all the benign tumors originating from the supportive tissue of various organs and the nonepithelial, extraskeletal structures (exclusive of lymphohematopoietic tissues) : fibrous connective tissue, adipose tissue, skeletal muscle, blood/lymph vessels, and the peripheral nervous system. Benign connective tissue tumors are 100 times more frequent than the malignant ones (sarcomas). Among these, the most frequent are: lipoma, hemangioma, leiomyoma, chondroma and osteoma.
Nomenclature : suffix "oma"+ type of the proliferated tissue.Chondroma Chondroma is a benign cartilaginous tumor, encapsulated, with a lobular growing pattern. Tumor cells (chondrocytes, cartilaginous cells) resemble normal cells and produce the cartilaginous matrix (amorphous, basophilic material). Characteristic are the vascular axes within the tumor, which make the distinction with normal hyaline cartilage. (H&E, ob. x10) Chondroma is a benign cartilaginous tumor, encapsulated, with a lobular growing pattern. Tumor cells (chondrocytes, cartilaginous cells) resemble normal cells and produce the cartilaginous matrix (amorphous, basophilic material). Characteristic are the vascular axes within the tumor, which make the distinction with normal hyaline cartilage. (H&E, ob. x10)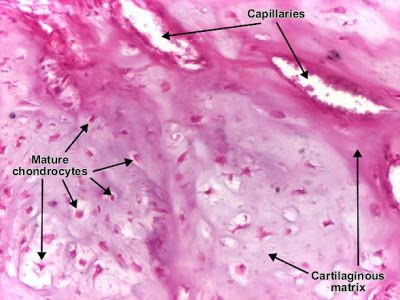 Chondroma. (H&E, ob. x40)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــCavernous hemangioma liver Chondroma. (H&E, ob. x40)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــCavernous hemangioma liver Cavernous hemangioma is a benign connective tissue tumor resulted from endothelial cells proliferation. It is a non-encapsulated tumor, with an infiltrative, lobular growing. The tumor consists in large (cavernous) spaces, lined by tumor endothelial cells (which appear very similar to normal cells). These interconnected spaces are filled with blood and separated by a fibrous tissue. (H&E, ob. 4) Cavernous hemangioma is a benign connective tissue tumor resulted from endothelial cells proliferation. It is a non-encapsulated tumor, with an infiltrative, lobular growing. The tumor consists in large (cavernous) spaces, lined by tumor endothelial cells (which appear very similar to normal cells). These interconnected spaces are filled with blood and separated by a fibrous tissue. (H&E, ob. 4) Cavernous hemangioma (liver). (H&E, ob. X10)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــLeiomyoma (uterus) Cavernous hemangioma (liver). (H&E, ob. X10)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــLeiomyoma (uterus) Uterine leiomyoma is a benign connective tissue tumor of the smooth muscle cells of the myometrium. Tumor cells resemble normal cells (uniform, elongated, spindle-shaped, with a cigar-shaped nucleus) and form bundles with different directions (whirled). The tumor may present areas of fibrosis, calcification and/or hemorrhage. The tumor is well circumscribed, but not encapsulated. (Hematoxylin-eosin, ob. x10)Patholgy Slides : Tumors or Neoplasia Malignant tumors of the connective tissue اضغط على الصورة للتكبير -ـ Click on image to enlarge sizeMalignant tumors of the connective tissue (sarcomas, from Greek sarkoma - "fleshy", because the gross aspect these tumors) are much more rare, comparing with carcinomas. Ninety percent of them are diagnosed in children and young adults, being localized mainly in lower extremities (40 %), retroperitoneum (30 %), upper extremities (20 %), head and neck (10 %). Uterine leiomyoma is a benign connective tissue tumor of the smooth muscle cells of the myometrium. Tumor cells resemble normal cells (uniform, elongated, spindle-shaped, with a cigar-shaped nucleus) and form bundles with different directions (whirled). The tumor may present areas of fibrosis, calcification and/or hemorrhage. The tumor is well circumscribed, but not encapsulated. (Hematoxylin-eosin, ob. x10)Patholgy Slides : Tumors or Neoplasia Malignant tumors of the connective tissue اضغط على الصورة للتكبير -ـ Click on image to enlarge sizeMalignant tumors of the connective tissue (sarcomas, from Greek sarkoma - "fleshy", because the gross aspect these tumors) are much more rare, comparing with carcinomas. Ninety percent of them are diagnosed in children and young adults, being localized mainly in lower extremities (40 %), retroperitoneum (30 %), upper extremities (20 %), head and neck (10 %).
Nomenclature : type of the tissue to which the malignant tumor will differentiate + "sarcoma".Fibrosarcoma Fibrosarcoma (fibroblastic sarcoma) is a malignant connective (soft) tissue tumor which originates from fibroblasts. The tumor may present different degrees of differentiation : low grade (differentiated), intermediate malignancy and high malignancy (anaplastic). The degree of differentiation is set according with: resemblance of tumor cell with mature fibroblast (spindle-shaped), amount of collagen secretion and mitotic rate. Tumor cells are arranged in short fascicles which split and merge, giving the appearance of "fish bone". Poorly differentiated tumors consist in more atypical cells, pleomorphic, giant cells, multinucleated, numerous atypical mitoses and reduced collagen production. Presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors the bloodstream metastasizing. (Hematoxylin-eosin, ob. X20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــOsteosarcoma (osteogenic sarcoma) Fibrosarcoma (fibroblastic sarcoma) is a malignant connective (soft) tissue tumor which originates from fibroblasts. The tumor may present different degrees of differentiation : low grade (differentiated), intermediate malignancy and high malignancy (anaplastic). The degree of differentiation is set according with: resemblance of tumor cell with mature fibroblast (spindle-shaped), amount of collagen secretion and mitotic rate. Tumor cells are arranged in short fascicles which split and merge, giving the appearance of "fish bone". Poorly differentiated tumors consist in more atypical cells, pleomorphic, giant cells, multinucleated, numerous atypical mitoses and reduced collagen production. Presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors the bloodstream metastasizing. (Hematoxylin-eosin, ob. X20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــOsteosarcoma (osteogenic sarcoma) 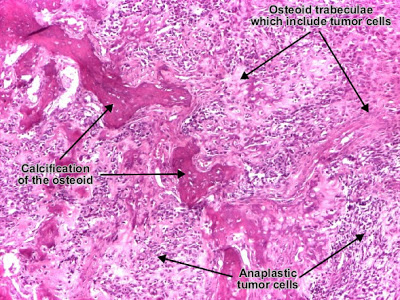 Osteosarcoma (osteogenic sarcoma) (H&E, ob. x10) Osteosarcoma (osteogenic sarcoma) (H&E, ob. x10) Osteosarcoma (osteogenic sarcoma) is a malignant tumor whose neoplastic cells present osteoblastic differentiation and form tumor bone. Tumor cells are very pleomorphic (anaplastic), some are giant and present numerous and atypical mitotic figures. These cells produce osteoid describing irregular trabeculae (amorphous, eosinophilic/pink) with or without central calcification (hematoxylinophilic/blue, granular) - tumor bone. Tumor cells are included in the osteoid matrix. Cartilage may be present. Presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors the bloodstream metastasizing. (Hematoxylin-eosin, ob. x10)Patholgy Slides : Tumors or Neoplasia Teratomas and Melanocytic tumors Osteosarcoma (osteogenic sarcoma) is a malignant tumor whose neoplastic cells present osteoblastic differentiation and form tumor bone. Tumor cells are very pleomorphic (anaplastic), some are giant and present numerous and atypical mitotic figures. These cells produce osteoid describing irregular trabeculae (amorphous, eosinophilic/pink) with or without central calcification (hematoxylinophilic/blue, granular) - tumor bone. Tumor cells are included in the osteoid matrix. Cartilage may be present. Presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors the bloodstream metastasizing. (Hematoxylin-eosin, ob. x10)Patholgy Slides : Tumors or Neoplasia Teratomas and Melanocytic tumors
اضغط على الصورة للتكبير -ـ Click on image to enlarge size
Teratomas
Benign microcystic teratoma of the ovary
ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Teratoma is a tumor which arises from tutipotent germinal cells. Frequently, it is localized in gonads (testis, ovary). It contains a variety of tissues (derived from one, two or three embryonic cell layers - mesoderm, endoderm or ectoderm), tissues which normally are foreign to the site of growth.

Mature teratoma (dermoid cyst) containing well-differentiated structures : respiratory epithelium and nervous tissue - brain. (H&E, ob. x10)
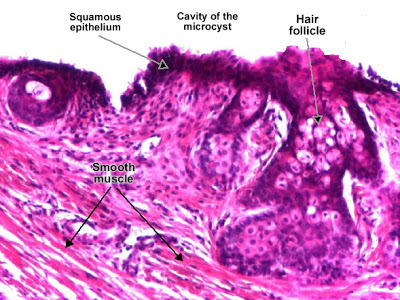
Benign microcystic teratoma of the ovary (II)
Mature teratoma (dermoid cyst) containing well-differentiated structures : respiratory epithelium, hair follicle and smooth muscle. (H&E, ob. x20)

Benign microcystic teratoma of the ovary (III)
Mature teratoma (dermoid cyst) containing well-differentiated structures : stratified epithelium, hair and fat tissue. (H&E, ob. x20)
ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Melanocytic tumors
Intradermal melanocytic nevus
Nevus cells (melanocytes) are normally localized in the basal layer of the epidermis. Their proliferation may appear in the epidermis (jonctional nevus), in the epidermis and dermis (compound nevus) or only in the dermis (intradermal nevus).

Intradermal melanocytic nevus - a benign tumor in which the tumor cells form nests in the dermis, are regular, round, with central nucleus and single nucleolus. In the supreficial dermis, some melanocytes may produce melanin pigment in the cytoplasm (dark-brown, granular). (H&E, ob.x4)
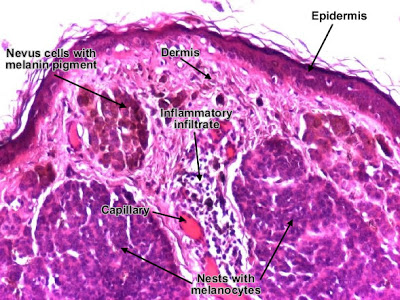
Intradermal melanocytic nevus (detail)
Intradermal melanocytic nevus (detail). (Hematoxilina-eozina, ob. x10) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:07 am الإثنين 19 نوفمبر 2018, 12:07 am | |
| Patholgy Slides : Hemodynamic derangements Edemaاضغط على الصورة للتكبير -ـ Click on image to enlarge sizeEdema represents the accumulation of excess liquid in the interstitial (extracellular) spaces of a tissue or in pre-existing cavities. It may affect any organ, but most often it appears in : subcutaneous tissues, lung and brain.
According to the etiology, edema may be localized (in inflammation or in impaired venous drainage) or systemic (in right heart failure or in nephrotic syndrome). A generalized and severe edema is called anasarca.
Accumulation of transudate or non-inflammatory fluid (effusions) in body cavities :
- Peritoneal cavity - ascites
- Pleural cavity - hydrothorax
- Pericardial cavity - hydropericardium
Pulmonary edemaEtiology of pulmonary edema : acute left heart (ventricular) failure, pulmonary failure in syndrome of adult respiratory distress, pulmonary infections and hypersensitivity reactions Pulmonary edema. Alveolar walls are thickened due to acute distention of capillaries and interstitial edema. Alveolar lumen is filled with transudate (pale-eosinophilic, finely granular), a liquid which replaces the air. (H&E, ob. x20) Pulmonary edema. Alveolar walls are thickened due to acute distention of capillaries and interstitial edema. Alveolar lumen is filled with transudate (pale-eosinophilic, finely granular), a liquid which replaces the air. (H&E, ob. x20) Pulmonary edema (detail)Patholgy Slides : Hemodynamic derangementsPassive congestion (Passive hyperemia) (lung) Pulmonary edema (detail)Patholgy Slides : Hemodynamic derangementsPassive congestion (Passive hyperemia) (lung)
اضغط على الصورة للتكبير -ـ Click on image to enlarge size
Hyperemia (congestion) represents the increase of blood in a territory, due to dilatation of small vessels. According to the mechanism, it may be active or passive.
Active hyperemia (congestion) is a result of arteriolar distension (e.g., skeletal muscle activity, inflammation, local neuro-vegetative reaction).
Passive hyperemia (congestion), also termed stasis, is a consequence of an impaired venous drainage (heart failure, compression or obstruction of veins), followed by dilatation of venules and capillaries
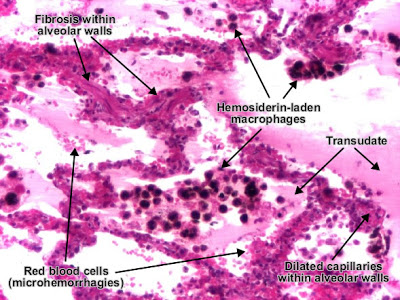
Etiology of passive congestion of the lung : chronic left heart (ventricular) failure.
Alveolar walls are thickened due to dilated capillaries. Alveolar lumens are filled with transudate (amorphous, eosinophilic and homogenous) which replaced the air, red blood cells (microhemorrhages) and hemosiderin-laden macrophages (also called "heart failure cells"). (H&E, ob. x20)
With progression, interstitial fibrosis may appear and, together with hemosiderin pigmentation, generates the aspect of "brown induration". Extensive fibrosis leads to intrapulmonary hypertension.
ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Passive congestion (Passive hyperemia) (lung) (detail)

Passive congestion of the lung. Hemosiderin-laden macrophages contain in cytoplasm hemosiderin pigment (brown, granular), resulted from destruction of red blood cells in alveolar lumen. (H&E, ob. x40)
Perls reaction is useful in distinguishing hemosiderin pigment from anthracotic (carbon) pigment : trivalent iron from hemosiderin stains in green-blue, while anthracotic pigment remains dark-brown and is mainly located perivascular. |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:08 am الإثنين 19 نوفمبر 2018, 12:08 am | |
| Patholgy Slides : Cardiovascular pathology
اضغط على الصورة للتكبير -ـ Click on image to enlarge size Coronary atherosclerosis - fibro fatty plaque Coronary artery with atherosclerosis (fibro-lipid or fibro-fatty plaque). The atheromatous fibro-fatty plaque is characterized by the accumulation of lipids in the intima of the arteries, narrowing the lumen and compressing the muscular layer. Beneath the endothelium it has a "fibrous cap" covering the atheromatous "core" of the plaque, which consists in cholesterol, cholesterol esters, fibrin, lipid-laden cells (macrophages and smooth muscle cells), proteoglycans, collagen, elastin and cellular debris. The cholesterol crystals form empty, needle-like clefts. At the periphery of the plaque are "foamy" cells and capillaries. (H&E, ob x4) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Coronary atherosclerosis - the fibrous plaque with calcification Coronary artery with atherosclerosis (fibrous plaque). The atheromatous fibrous plaque is localized in the intima of the artery, beneath the endothelium, producing the thickening of the wall and, secondary, the narrowing of the lumen and the atrophy of the muscular layer by compression. The fibrous plaque contains collagen fibres (eosinophilic), precipitates of calcium(hematoxylinophilic) and rare lipid-laden cells. (H&E, ob. x4) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Recent coronary thrombosis Thrombosis : recent thrombus in a coronary artery (branch in the epicardium) : The arterial lumen is completely obstructed by a recent thrombus - fibrin network (pink) containing red blood cells and platelets. The thrombus is developed on an ulcerated atherosclerotic (fibrous) plaque and is adherent to the arterial wall. (H&E, ob. x4) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Acute myocardial infarct Myocardial infarct - circumscribed area of ischemic necrosis - coagulative necrosis. In the first 12 - 24 hours, myocardial fibers are still well delineated, with intense eosinophilic (pink) cytoplasm, but lost their transversal striations and the nucleus (left side of the picture). Notice a few myocardial fibers showing hypertrophy (increased size of the fiber, irregular shape of the nuclei). (H&E, ob. x20) Recent myocardial infarct (in the first 12 - 24 hours): myocardial fibers are still well delineated, with intense eosinophilic (pink) cytoplasm, but lost their transversal striations and the nucleus. The interstitial space may be infiltrated with red blood cells. Make the distinction between interstitial leucocytes (small, outside the myocardial fibers) and the myocardial nucleus (should be central and unique, but is absent here) ! (H&E, ob. x10) Recent myocardial infarct (first 24 hours) (detail). (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Myocardial infarct healing Myocardial infarct (healing commencing) - between 5th and 10th day. In area of coagulative ischemic necrosis, myocardial fibers preserve their contour, but the cytoplasm is intensely eosinophilic and transversal striations and nuclei are lost. The interstitium of the infarcted area is initially infiltrated with neutrophils, then with lymphocytes and macrophages, in order to fagocitate the myocyte debris. The necrotic area is surrounded and progressively invaded by granulation tissue which will replace the infarct with a fibrous (collagenous) scar. (H&E, ob. x4, multifield digitally composed picture) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Hyaline arteriolosclerosis (Benign nephrosclerosis) In benign hypertension, hyaline (pink, amorphous, homogeneous material) accumulates in the wall of small arteries and arterioles, producing the thickening of their walls and the narrowing of the lumens. Consequent ischemia will produce tubular atrophy, interstitial fibrosis, glomerular alterations (smaller glomeruli with different degrees of hyalinization - from mild to sclerosis of glomeruli) and periglomerular fibrosis. (Hematoxylin-eosine, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Acute viral myocarditis Myocarditis is an inflammation of the myocardium. Acute viral myocarditis is produced most often by Coxsackie B virus and echovisuses. Myocardial interstitium presents an abundant edema and inflammatory infiltrate, mainly with lymphocytes and macrophages. Focal destruction of myocytes may be present, generating loss of contractile function of the myocardium. (H&E, ob. x10) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Ischemic fibrosis of myocardium (diffuse ventricular myocardial fibrosis) Diffuse myocardial fibrosis (Ischemic fibrosis of the myocardium) (Simionescu trichromic staining, ob. x4) : myocardial cells (red) intermingled with collagen-rich fibrosis (blue) which completely replaced the necrotic myocardial cells. Capillaries (with yellow-orange red blood cells) within fibrosis remained from repair by connective tissue process. Diffuse myocardial fibrosis (Ischemic fibrosis of the myocardium) (Simionescu trichromic staining, ob. x10) : viable myocardial cells (red) with nuclei (brown) surrounded by collagen-rich fibrosis (blue). Fibrosis completely replaced the necrotic myocardial cells. Capillaries (with yellow-orange red blood cells) within fibrosis remained from repair by connective tissue process. |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:08 am الإثنين 19 نوفمبر 2018, 12:08 am | |
| Patholgy Slides : Pulmonary pathology
اضغط على الصورة للتكبير -ـ Click on image to enlarge size Edema Edema represents the accumulation of excess liquid in the interstitial (extracellular) spaces of a tissue or in pre-existing cavities. It may affect any organ, but most often it appears in : subcutaneous tissues, lung and brain.
According to the etiology, edema may be localized (in inflammation or in impaired venous drainage) or systemic (in right heart failure or in nephrotic syndrome). A generalized and severe edema is called anasarca.
Accumulation of transudate or non-inflammatory fluid (effusions) in body cavities :
- Peritoneal cavity - ascites
- Pleural cavity - hydrothorax
- Pericardial cavity - hydropericardium
Pulmonary edema Etiology of pulmonary edema : acute left heart (ventricular) failure, pulmonary failure in syndrome of adult respiratory distress, pulmonary infections and hypersensitivity reactions Pulmonary edema. Alveolar walls are thickened due to acute distention of capillaries and interstitial edema. Alveolar lumen is filled with transudate (pale-eosinophilic, finely granular), a liquid which replaces the air. (H&E, ob. x20)
Pulmonary edema (detail) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Passive congestion (Passive hyperemia) (lung) Hyperemia (congestion) represents the increase of blood in a territory, due to dilatation of small vessels. According to the mechanism, it may be active or passive. Active hyperemia (congestion) is a result of arteriolar distension (e.g., skeletal muscle activity, inflammation, local neuro-vegetative reaction).
Passive hyperemia (congestion), also termed stasis, is a consequence of an impaired venous drainage (heart failure, compression or obstruction of veins), followed by dilatation of venules and capillaries. Etiology of passive congestion of the lung : chronic left heart (ventricular) failure.
Alveolar walls are thickened due to dilated capillaries. Alveolar lumens are filled with transudate (amorphous, eosinophilic and homogenous) which replaced the air, red blood cells (microhemorrhages) and hemosiderin-laden macrophages (also called "heart failure cells"). (H&E, ob. x20)
With progression, interstitial fibrosis may appear and, together with hemosiderin pigmentation, generates the aspect of "brown induration". Extensive fibrosis leads to intrapulmonary hypertension.
Passive congestion (Passive hyperemia) (lung) (detail)  Passive congestion of the lung. Hemosiderin-laden macrophages contain in cytoplasm hemosiderin pigment (brown, granular), resulted from destruction of red blood cells in alveolar lumen. (H&E, ob. x40)
Perls reaction is useful in distinguishing hemosiderin pigment from anthracotic (carbon) pigment : trivalent iron from hemosiderin stains in green-blue, while anthracotic pigment remains dark-brown and is mainly located perivascular. ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Hemorrhagic infarct lung Pulmonary infarct (hemorrhagic infarct of the lung) is an area of ischemic necrosis produced by venous thrombosis on a background of passive congestion of lung. In infarct area, alveolar walls, vascular walls and bronchioles are necrotic. They appear eosinophilic (pink), homogenous, lacking the nuclei, but keep their shapes - "structured necrosis". Alveolar lumens from infarcted area are invaded by red blood cells - hemorrhagic infarct (red). (H&E, ob. x10)
Hemorrhagic infarct lung (detail) Pulmonary infarct in an area of passive congestion. The hemosiderin-laden macrophages present inside the alveolar lumen are witnesses of pre-existent passive congestion. (H&E, ob. x20)
Hemorrhagic infarct lung venous thrombosis ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Lobar pneumonia (leukocytic alveolitis) Lobar pneumonia is an acute exudative inflammation of an entire pulmonary lobe, produced in 95 % of cases by Streptococcus pneumoniae (pneumococci). If not treated, lobar pneumonia evolves in four stages :
Congestion (first 2 days)
Red hepatisation (fibrinous alveolitis) (2nd to 4th day)
Grey hepatisation (leukocytic alveolitis) (4th to 8th day)
[*] Resolution (after 8th day) Leukocytic alveolitis is the 3rd phase of the lobar pneumonia. Alveolar lumens are filled with leukocytic (suppurative) exudate (neutrophils and macrophages, in order to remove the fibrin). Alveolar walls are thickened due to capillary congestion and edema. (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Bronchopneumonia (Lobular pneumonia) Bronchopneumonia (Lobular pneumonia) is an acute exudative inflammation of the lungs characterised by foci of consolidation surrounded by normal parenchyma. Usually, bronchopneumonia affects one or more lobes and is bilateral. Bronchopneumonia : focus of inflammatory condensation centred by a bronchiole with acute bronchiolitis (suppurative exudate in the lumen and parietal inflammation). Alveolar lumens surrounding the bronchia are filled with neutrophils ("leukocytic alveolitis"). Inflammatory foci are separated by normal, aerated parenchyma. (H&E, ob. x10) Bronchopneumonia (detail) : central area of a focus of inflammatory condensation - bronchiola with acute bronchiolitis. (H&E, ob. X20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Aspiration bronchopneumonia Aspiration bronchopneumonia appears when early respiratory movements during labor, facilitate filling of alveolar ducts and alveolar lumens with elements of amniotic fluid : amniotic cells, squames and squamous cells from fetal skin, lanugo, meconium. Reduced inflammatory infiltrate (neutrophils) and capillary congestion is present. (H&E, ob. x20) Aspiration bronchopneumonia with amniotic fluid. (H&E, ob. x20) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Pulmonary tuberculosis Tuberculosis is a chronic inflammation caused by Mycobacterium tuberculosis (tubercle bacillus, Koch bacillus) - human type or bovine type. The most affected organ by tuberculosis is the lung. Microscopically, the characteristic lesion in tuberculosis is the tuberculous granuloma Pulmonary tuberculosis. Tuberculous granuloma is localized in the pulmonary interstitium, compressing the surrounding alveoli and destroing the parenchyma. (Hematoxylin-eosin, ob. x4) (For detailed histological description of granuloma
Pulmonary tuberculosis (detail 1) Tuberculous granuloma in the pulmonary interstitium. (Hematoxylin-eosin, ob. X20)
Pulmonary tuberculosis (detail 2)
Tuberculous granuloma in the pulmonary interstitium. (Hematoxylin-eosin, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Pneumoconiosis - Silicosis Silicosis is a pneumoconiosis produced by chronic exposure to silica dust (workers in glass industry, sand blasters, miners, grinders and polishers, cement workers). After inhalation, silica particles are phagocytated by macrophages which shortly after die and so, the released silica particles will be phagocytated by other macrophages. These macrophages seems to secrete a fibroblast grown factor which stimulates the fibrosis. Pulmonary silicosis. Continuous accumulation of collagen around inhaled silica crystals produces pulmonary fibrotic hyalinized (silicotic) nodules. They present concentric laminated collagen fibers (blue) and tend to become confluent, compressing adjacent alveoli. Silica crystals appear as empty cleft-like spaces. With progression, perivascular and peribronchiolar collagen deposits will produce pulmonary hypertension. (Simionescu trichromic staining, ob. x4) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Neonatal respiratory distress syndrome - NRDS (Hyaline membrane disease) Neonatal Respiratory Distress Syndrome - NRDS (Hyaline membrane disease) is characterized by collapsed alveoli alternating with hyperaerated alveoli, vascular congestion and hyaline membranes (resulted from fibrin, cellular debris, red blood cells). Hyaline membranes appear like an eosinophilic, amorphous material, lining or filling the alveolar spaces and blocking the gases exchange. (H&E, ob. x10)
Hyaline membrane disease (detail 1)
Hyaline membrane disease. (H&E, ob. x40)
Hyaline membrane disease (detail 2) Hyaline membrane disease. (H&E, ob. x40) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:09 am الإثنين 19 نوفمبر 2018, 12:09 am | |
| Patholgy Slides : Gastrointestinal tract pathology
اضغط على الصورة للتكبير -ـ Click on image to enlarge size Stomach ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Chronic gastritis with Helicobacter Pylori Chronic gastritis associated with infection with Helicobacter pylori.
Helicobacter pylori (blue bars, curved, 2 - 4 microns) rims in the mucus on the mucosa surface, at the intercellular lines. Photo : tangential section of the gastric mucosa. (Giemsa, ob. x40) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Chronic peptic ulcerChronic peptic ulcer (stomach) is a mucosal defect which penetrates the muscularis mucosae and muscularis propria, produced by acid-pepsin aggression. Ulcer margins are perpendicular and present chronic gastritis. During the active phase, the base of the ulcer shows 4 zones : inflammatory exudate, fibrinoid necrosis, granulation tissue and fibrous tissue. The fibrous base of the ulcer may contain vessels with thickened wall or with thrombosis. (H&E, ob. x7) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Chronic peptic ulcer (detail) Chronic peptic ulcer (stomach). During the active phase, the base of the ulcer shows 4 zones :
- inflammatory exudate - at the lumen (cell debris and neutrophils)
- fibrinoid necrosis (yellow in van Gieson staining and pink in H&E)
- granulation tissue (see Granulation tissue)
- mature fibrous tissue (abundant collagen - red in van Gieson staining and pink in H&E, profound, spreading beneath ulcers margins, producing mucosal retraction - radiating folds). This fibrous layer may contain vessels with thickened walls or with thrombosis. (H&E, ob. x10)
ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Gastric carcinoma, intestinal typeGastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, intestinal type. Tumor cells describe irregular tubular structures, with stratification, multiple lumens surrounded by a reduced stroma ("back to back" aspect). The tumor invades the gastric wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Often it associates intestinal metaplasia in adjacent mucosa. Depending on glandular architecture, cellular pleomorphism and mucosecretion, adenocarcinoma may present 3 degrees of differentiation : well (photo), moderate and poorly differentiate. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type, infiltrating muscularis propria. (H&E, ob. x10) Gastric adenocarcinoma, intestinal type. (H&E, ob. X40) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Gastric carcinoma, diffuse type (mucinous)Gastric adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the gastric mucosa. According to Lauren classification, gastric adenocarcinoma may be: intestinal type, diffuse type and mixed type. Gastric adenocarcinoma, diffuse (infiltrative) type. Tumor cells are discohesive and secrete mucus which is delivered in the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated (Lauren classification). If the mucus remains inside the tumor cell, it pushes the nucleus against the cell membrane - "signet-ring cell". (H&E, ob. x10) Gastric carcinoma, diffuse type (mucinous) - detail Gastric adenocarcinoma, diffuse type. (H&E, ob. X20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Colonــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Adenomatous tubulo-villous polyp, pedunculated (colon)Adenoma is a benign epithelial tumor arising in epithelium of mucosa (stomach, small intestine and bowel), glands (endocrine and exocrine) and ducts. In hollow organs (e.g. digestive tract) the adenoma grows upwards into the lumen - adenomatous polyp or polypoid adenoma. Depending on the type of the insertion base, adenoma may be pedunculated (lobular head with a long, slender stalk, covered by normal mucosa - see photo) or sessile (broad base). If not elevated above the surface of the mucosa, the adenoma is called flat adenoma. 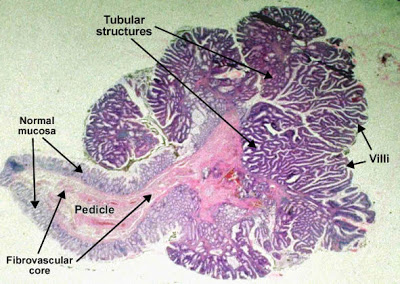 Adenomatous tubulo-villous polyp, pedunculated (colon). The adenomatous proliferation is characterized by different degrees of cell dysplasia (cellular and architectural atypia) : loss of normal differentiation of epithelium, irregular cells with hyperchromatic nuclei, (pseudo)stratified nuclei, nucleolus, decreased mucosecretion and mitosis. The architecture may be tubular, villousor tubulo-villous. Basement membrane and muscularis mucosae are intact. (HE, ob. x4) Detail of an adenomatous tubulo-villous polyp (colon) Compared to normal colonic epithelium (lower left corner of the picture) the adenomatous proliferation is characterized by different degrees of cell dysplasia and tubular, villous or tubulo-villousarchitecture. In tubular component tumor cells proliferate generating tubular shapes, more or less irregular or branched. The villous pattern presents villi - finger-like projections lined by dysplastic epithelium and with thin fibro-vascular core. Passage from tumoral epithelium to normal mucosa is abrupt. (HE, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Adenomatous villous polyp, sessile (colon)Adenoma is a benign epithelial tumor arising in epithelium of mucosa (stomach, small intestine and bowel), glands (endocrine and exocrine) and ducts. In hollow organs (e.g. digestive tract) the adenoma grows upwards into the lumen - adenomatous polyp or polypoid adenoma. Depending on the type of the insertion base, adenoma may be pedunculated (lobular head with a long, slender stalk, covered by normal mucosa) or sessile (broad base - see photo). If not elevated above the surface of the mucosa, the adenoma is called flat adenoma. Adenomatous villous polyp, sessile (colon). The adenomatous proliferation is characterized by different degrees of cell dysplasia(cellular and architectural atypia) : loss of normal differentiation of epithelium, irregular cells with hyperchromatic nuclei, (pseudo)stratified nuclei, nucleolus, decreased mucosecretion and atypical mitosis. The architecture may be tubular, villous (photo) or tubulo-villous. Basement membrane and muscularis mucosae are intact. (HE, ob. x4) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Moderately differentiated adenocarcinoma (colon)Adenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa (photo) and thence the muscularis propria. (Notice the end-point of muscularis mucosae. At left from this point, muscularis mucosae is continuous. At right from this point, muscularis mucosae is destroyed by tumor cells invasion.) Tumor cells describe irregular tubular structures, harboring stratification, multiple lumens, reduced stroma ("back to back" aspect). Depending on glandular architecture, cellular pleomorphism and mucosecretion of the predominant pattern, adenocarcinoma may present 3 degrees of differentiation: well, moderate and poorly differentiate. (H&E, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Poorly differentiated adenocarcinoma (mucinous), colonAdenocarcinoma is a malignant epithelial tumor, originating from glandular epithelium of the colorectal mucosa. It invades the wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Tumor cells are discohesive and secrete mucus which invades the interstitium producing large pools of mucus/colloid (optically "empty" spaces) - mucinous (colloid) adenocarcinoma, poorly differentiated. If the mucus remains inside the tumor cell, it pushes the nucleus at the periphery, against the cell membrane - "signet-ring cell". (H&E, ob. x20) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:10 am الإثنين 19 نوفمبر 2018, 12:10 am | |
| Patholgy Slides : Liver, Biliary Tract and Pancreas اضغط على الصورة للتكبير -ـ Click on image to enlarge size Liver Liver diseases with toxic (alcoholic or chemical) or viral etiology (hepatitis B, C or D virus) very often are the cause of cirrhosis. Independent of its' etiology, cirrhosis is considered to be a premalignant lesion for primary liver cancer (hepatocellular carcinoma). Nonetheless, about 95% of all liver cancers are secondary determinations (liver metastasis of other tumors). Cholecystitis is the most frequent disease of the gallbladder. Non-tumor pathology of the pancreas refers to acute hemorrhagic pancreatitis and chronic pancreatitis. Although it is the fifth as incidence among other cancers, carcinoma of the pancreas has an extremely severe prognosis Fatty change (liver) - Steatosis Fatty change or Steatosis represents the intracytoplasmic accumulation of triglyceride (neutral fats) of parenchimal organs, such as: liver, myocardium and kidney. Mechanisms : increase of free fatty acids (starvation, diabetes and chronic ethylism/alcoholism), reduction of free fatty acids oxidation (hypoxia, toxins, chronic ethylism/alcoholism), increase of esterification of free fatty acids into triglycerides (due to increased free fatty acids or reduction of their oxidation, chronic ethylism/alcoholism) and reduced export of tryglicerides due to deficiency of lipid binding apoprotein (starvation/malnutrition, toxins). Initially, fatty change does not impair the cells function, being reversible. At the beginning, the hepatocytes present small fat vacuoles in the vicinity of the endoplasmic reticulum (liposomes) - microvesicular fatty change (photo). In the late stages, the size of the vacuoles increases pushing the nucleus to the periphery of the cell - macrovesicular fatty change. These vesicles are well delineated and optically "empty" because fat solves during tissue processing (paraffin embedding). Large vacuoles may coalesce, producing fatty cysts - which are irreversible lesions. (HE, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Viral chronic moderate hepatitis Chronic hepatitis is characterized by hepatic necroinflammation (chronic inflammatory infiltrate and necrosis of hepatocytes), fibrosis and biochemical disorders lasting for more than 6 months. According to necroinflammatory activity, chronic hepatitis may be mild, moderate or severe. The stage of fibrosis depends on its' localization and degree of extension (absent, limited to portal tract without fibrous septa, complete or incomplete porto-portal fibrous septa and cirrhosis).
The main cause chronic hepatitis is viral infection : hepatitis B virus, hepatitis C virus, and others. Untreated, chronic viral hepatitis evolves into cirrhosis and hepatocellular carcinoma.  In moderate chronic hepatitis, the liver architecture is preserved, but portal tracts are enlarged (losing the normal triangular shape), with abundant chronic inflammatory infiltrate (lymphocytes, plasma cells, macrophages). Limiting plate of hepatocytes (which separates the portal tract from lobule) is interrupted (foci of hepatocyte necrosis surrounded by lymphocytes - piecemeal necrosis or interface hepatitis). This is followed by extension of inflammation into the periportal parenchyma. At this level, hepatocytes present hydropic change and/or fatty change. (H&E, ob. x20)
ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Secondary biliary cirrhosis Secondary biliary cirrhosis is produced by obstruction of extrahepatic biliary ducts and is characterized by regeneration nodules, surrounded by fibrous septa. In these nodules, regenerating hepatocytes are disorderly disposed. Biliary tract, central vein and the radiar pattern of hepatocytes are absent. Fibrous septa are important and may present inflammatory infiltrate (lymphocytes, macrophages) and biliary ducts (damaged, proliferated or distended - bile stasis). These dilated ducts contain inspissated bile which appear as bile casts or bile thrombi (brown-green, amorphous). Bile retention may be found also in the parenchyma, as the so called "bile lakes". (H&E, ob. x10)
Secondary biliary cirrhosis (detail)
Regeneration nodule in secondary biliary cirrhosis. (H&E, ob. x40) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Poorly differentiated hepatocellular carcinoma Hepatocellular carcinoma, poorly differentiated (photo - upper right), developed on liver cirrhosis. This malignant epithelial tumor consists in tumor cells, discohesive, pleomorphic, anaplastic, giant. The tumor has a scant stroma and central necrosis because of the poor vascularization. In well differentiated forms, tumor cells resemble hepatocytes, form cords and nests, and may contain bile pigment in cytoplasm. (H&E, ob. x20) Poorly differentiated hepatocellular carcinoma. (H&E, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Biliary Tract Cholesterolosis (strawberry gallbladder) Cholesterolosis is an intracellular accumulation of lipids (cholesterol). When cholesterol is in excess in the bile, it passes into the lamina propria where is phagocitated by macrophages. These macrophages become larger and polygonal, with foamy cytoplasm and small, hyperchromatic, central nucleus (xantic cells). Aggregation of xantic cells may enlarge the mucosal folds, producing a polypoid appearance of the mucosal surface. At gross examination, these yellow micropolyps (1-2 mm) contrasts with the red aspect of the surrounding mucosa, hence the term "strawberry gallbladder". Sometimes, cholesterolosis is associated with inflammation of the gallbladder (cholecystitis) or with gallstones (cholelithiasis). Cholesterolosis of the gallbladder. (HE, ob x4) Cholesterolosis of the gallbladder (detail of an enlarged mucosal fold). (HE, ob x10) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Pancreas Acute pancreatitis (Acute hemorrhagic pancreatic necrosis) The acute pancreatitis (acute hemorrhagic pancreatic necrosis) is characterized by acute inflammation and necrosis of pancreas parenchyma, focal enzyme necrosis of pancreatic fat and vessels necrosis - hemorrhage. These are produced by intrapancreatic activation of pancreatic enzymes. Lipase activation produces the necrosis of fat tissue in pancreatic interstitium (photo) and peripancreatic spaces. Necrotic fat cells appear as shadows, contours of cells, lacking the nucleus, pink, finely granular cytoplasm. It is possible to find calcium precipitates (hematoxylinophilic). Digestion of vascular walls results in thrombosis and hemorrhage. Inflammatory infiltrate is rich in neutrophils. (H&E, ob.x10)
Acute pancreatitis (Acute hemorrhagic pancreatic necrosis) (detail)
The acute pancreatitis (acute hemorrhagic pancreatic necrosis). Area of fat tissue necrosis due to lipase activation in the pancreatic interlobular space. The adjacent vessel presents thrombosis and hemorrhage. (H&E, ob.x40) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:10 am الإثنين 19 نوفمبر 2018, 12:10 am | |
| Pathology Slides : Kidney Patholoy اضغط على الصورة للتكبير -ـ Click on image to enlarge size
Depending on the affected segment, non-tumor nephropathies can be divided into : glomerular and tubulo-interstitial nephropaties. Primary glomerulonephritis :
acute diffuse proliferative glomerulonephritis (nephritic syndrome) rapidly progressive (crescentic) glomerulonephritis
lipoid nephrosis (minimal change disease) (nephrotic syndrome)
membranous glomerulonephritis (membranous nephropathy) (nephrotic syndrome)
membranoproliferative glomerulonephritis (nephrotic syndrome)
focal segmental glomerulosclerosis (nephrotic syndrome)
IgA nephropathy (Berger's disease)
chronic glomerulonephritis
Secondary glomerulonephritis may appear during some systemic diseases, such as: systemic lupus erythematosus, diabetes mellitus, amyloidosis, Goodpasture's syndrome, polyarteritis nodosa, Wegener's granulomatosis, Henoch-Schonlein purpura, bacterial endocarditis.
Tubulo-intestitial nephropaties are represented by : acute tubular necrosis (nephrotoxic or ischemic), inflammatory lesions of the tubules and interstitium (acute and chronic pyelonephritis, interstitial nephritis, including drug-induced interstitial nephritis).
Renal tumors are : benign (cortical adenoma, fibroma, angiomyolipoma, oncocytoma, urothelial papilloma) and malignant (renal cell carcinoma - Grawitz tumor, nephroblastoma - Wilms' tumor, urothelial carcinoma, sarcomas).
............................................................................................................. Poststreptococcal acute diffuse proliferative glomerulonephritis Acute postinfectious (poststreptococcal) diffuse proliferative glomerulonephritis is a primary glomerulonephritis, which produces nephritic syndrome (hematuria, oliguria, uremia, hypertension and mild proteinuria).
- "Acute" - because it occurs 2 weeks after a streptococcal (group A beta-hemolytic) pharyngitis. It becomes chronic only in 10 - 15 % of cases, especially in adults.
- "Diffuse" - because almost all the glomeruli are affected (about 80 %).
- "Proliferative" - due to proliferation of endothelial cells and mesangial cells.
The mechanism of poststreptococcal acute diffuse proliferative glomerulonephritis is immune : granular deposits of IgG and C3 ("humps") on the external (subepithelial) side of the basement glomerular membrane. These humps can be seen in electron microscopy and immunofluorescence microscopy. Acute postinfectious diffuse proliferative glomerulonephritis. Almost all glomeruli are enlarged (hypercellular) due to proliferation of endothelial cells and mesangial cells, swelling of endothelial cells and inflammatory infiltrate (neutrophils and monocytes). This will result in compression of capillaries and Bowman space, which is reduced in size. Initially, tubules are not affected, but with evolution, they may present hydropic change. (H&E, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Rapidly progressive ("crescentic") glomerulonephritis Rapidly progressive ("crescentic") glomerulonephritis is a primary glomerulonephritis, which produces nephritic syndrome (hematuria, oliguria, uremia, hypertension and mild proteinuria). The prognosis is severe, with rapid and irreversible evolution to renal failure. Etiology of rapidly progressive crescentic glomerulonephritis : streptococcal infection, systemic lupus, vasculitis, Goodpasture's syndrome, idiopathic. Rapidly progressive ("crescentic") glomerulonephritis - the majority of glomeruli present "crescents". Formation of crescents is initiated by passage of fibrin into the Bowman space as a result of increased permeability of glomerular basement membrane. Fibrin stimulates the proliferation of parietal cells of Bowman capsule, and an influx of monocytes. Rapid growing and fibrosis of crescents compresses the capillary loops and decreases the Bowman space which leads to renal failure within weeks or months. (H&E, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Chronic glomerulonephritis Chronic glomerulonephritis represents the end-stage of all glomerulonephritis with unfavorable evolution. This general (glomerular, vascular and interstitial) affection constitutes the so-called "end stage kidney". In most cases, it is associated with systemic hypertension.  Chronic glomerulonephritis. The majority of the glomeruli are affected. Depending on the stage of the disease, they may present different degrees of hyalinization (hyalinosclerosis - total replacement of glomeruli and Bowmann's space with hyaline). The hyaline is an amorphous material, pink, homogenous, resulted from combination of plasma proteins, increased mesangial matrix and collagen. Totally hyalinised glomeruli are atrophic (smaller), lacking capillaries, hence these glomeruli are non-functional. Few glomeruli may still present changes which permit to discern the etiology of chronic glomerulonephritis. Obstruction of blood flow will produce secondary tubular atrophy, interstitial fibrosis and thickening of the arterial wall by hyaline deposits. In the interstitium is present an abundant inflammatory infiltrate (mostly with lymphocytes). (Hematoxylin-eosine, ob. x20)   Chronic glomerulonephritis. Functional nephrons have dilated tubules, often with hyaline casts in the lumens. (Hematoxylin-eosine, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Diabetic glomerulosclerosis In diabetes, basement membranes of majority of capillaries in the body are thickened by deposits of nonenzymatic glycosilated proteins (diabetic microangiopathy): retinopathy, coronary arteries, and peripheral vessels.
In kidney, diabetic nephropathy includes : diabetic glomerulosclerosis, arteriolosclerosis and papillary necrosis, with an increased risk for pyelonephritis. Diabetic glomerulosclerosis is characterized by thickening of glomerular basement membrane with increased permeability. With time, the mesangial space becomes larger by deposits of proteins (collagen IV), initially diffuse, then nodular. Diffuse diabetic glomerulosclerosis. The deposits appear diffusely on the basement membranes of capillary loops of the glomeruli, as well as on basement membranes of tubules and arterioles. (PAS, ob. x40) In nodular diabetic glomerulosclerosis, PAS-positive nodular deposits (containing mucopolysaccharides, fibrils and collagen) may appear in the mesangial space, at the periphery of the glomerulus, pushing the capillaries. The lesion is focal (glomeruli are not entirely affected), and some of them are spared. This pattern is also called Kimmelstiel-Wilson lesion. (PAS, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Amyloidosis (kidney) Amyloid (an abnormal protein) accumulates as extra-cellular deposits, nodular or diffuse, as pink, amorphous material. Initially, the deposits appear in the glomeruli: within the mesangial matrix and along the basement membranes of the capillary loops. Continuous accumulation of the amyloid will compress and obliterate the capillary tuft. With progression, amyloid deposits appear also peritubular and within the arteriolar wall, narrowing them. Congo red is a special staining, elective for amyloid. (Congo Red, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Toxic tubular necrosis Acute tubular necrosis is a pathological entity characterized by destruction of tubular epithelial cells, followed by acute renal failure (oliguria, proteinuria, blood retention of urea and creatinine). Depending on etiology, there are two types of acute tubular necrosis :
toxic acute tubular necrosis, after ingestion or inhalation of toxic substance ethylene glycol, mercury, lead, carbon tetrachloride, methyl alcohol, nephrotoxic drugs
ischemic acute tubular necrosis - in shock
Toxic acute tubular necrosis is characterized by proximal tubular epithelium necrosis (no nuclei, intense eosinophilic homogenous cytoplasm, but preserved shape) due to interference of ingested toxic agents (poisons, organic solvents, drugs, heavy metals) with epithelial cell metabolism. Necrotic cells fall into the tubule lumen, obliterating it, and determining acute renal failure (oligo-anuria). Basement membrane is intact, so the tubular epithelium regeneration is possible, if the patient survives. The interstitium and glomeruli are not affected. (H&E, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Acute pyelonephritis Acute pyelonephritis is an exudative purulent localized inflammation of kidney and renal pelvis. The renal parenchyma presents in the interstitium abscesses (suppurative necrosis), consisting in purulent exudate (pus): neutrophils, fibrin, cell debris and central germ colonies (hematoxylinophils). Tubules are damaged by exudate and may contain neutrophil casts. In the early stages, glomeruli and vessels are normal. (Hematoxylin-eosine, ob. x10) Acute pyelonephritis (Hematoxylin-eosine, ob. x10) ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Nephroblastoma (Wilms' Tumor) Wilms' tumor (nephroblastoma) is a malignant mixed tumor containing metanephric blastema, stromal and epithelial derivatives. It is the most frequent renal tumor in children before age of 5 years (peak of incidence: 2 year-old). Etiology of Wilms' tumor (nephroblastoma) : mutations of WT1 gene on chromosome 11 and nephroblastematosis (persistence of renal blastema in kidney tissue). Wilms' tumor (nephroblastoma). The tumor consists in tumor epithelial component (abortive tubules and glomeruli) surrounded by metanephric blastema and tumor immature spindled cell stroma. The stroma may include differentiated (muscle, cartilage, bone, fat tissue, fibrous tissue) or anaplastic elements. The tumor (photo, left) compresses the normal kidney parenchyma ( photo, right) (H&E, ob. x10)
Nephroblastoma (Wilms' Tumor) (detail)
Wilms' tumor (nephroblastoma) : metanephric blastema, stromal and epithelial components. (H&E, ob. x20) ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ Renal cell carcinoma (Grawitz tumor) Renal clear cell carcinoma (Grawitz tumor) is a malignant epithelial tumor resulted from proliferation of tubule cells. Tumor cells form cords, papillae, tubules or nests, and are atypical, polygonal and large. Because these cells accumulate glycogen and lipids, their cytoplasm appears "clear", lipid-laden, the nuclei remain in the middle of the cells, and the cellular membrane is evident. Some cells may be smaller, with eosinophilic cytoplasm, resembling normal tubular cells. The stroma is reduced, but well vascularized. The tumor grows in large front, compressing the surrounding parenchyma, producing a pseudocapsule. (H&E, ob. x20) |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:11 am الإثنين 19 نوفمبر 2018, 12:11 am | |
| Pathology Slides : Hematopathology اضغط على الصورة للتكبير -ـ Click on image to enlarge sizeLymphomas are malignant proliferations of the lymphoid tissue, mainly of the lymph node; rarely, they can be extranodal (thymus, spleen, and mucosal associated lymphoid tissue - MALT lymphomas).There are two major types of lymphomas :Hodgkin's lymphomaNon-Hodgkin's lymphomaLeukemias are malignant proliferations of the hematopoietic stem cells in the bone marrow.
...........................................................................................................Chronic lymphoid leukemia (liver)Leukemia is a monoclonal malignant proliferation of stem cells of bone marrow, with replacement of normal bone marrow by leukemic cells, accumulation in peripheral blood and infiltration of organs (i.e., lymph nodes, spleen, liver, kidney). As a result of bone marrow infiltration, one or all series are suppressed, generating pancytopenia (anemia, neutropenia and thrombocytopenia).Leukemia classification, based upon clinical and histogenetic criteria :
- Acute leukemias (proliferation of young, immature elements)
- Lymfoblastic
- Myeloblastic
Chronic leukemias (monoclonal proliferation of non-functional lymphoid and myeloid elements)
Lymphocytic (lymphoid)
Granulocytic (myeloid)
Chronic lymphocytic (lymphoid) leukemia is a malignant lymphoid proliferation, similar to a low-grade lymphoma, but affecting mainly the bone marrow and the peripheral blood. Chronic lymphocytic (lymphoid) leukemia (liver). Tumor lymphocytic infiltrate into the portal tracts, which appear very enlarged, lacking normal structures. These tumor lymphoid cells resemble normal lymphocytes (small, monomorphic, round hyperchromatic homogenous nuclei, reduced cytoplasm), but are immature, monoclonal and non-functional. With evolution, the tumor cells will infiltrate the lobules. (H&E, ob. x10)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــChronic myeloid leukemia (liver)Leukemia is a monoclonal malignant proliferation of stem cells of bone marrow, with replacement of normal bone marrow by leukemic cells, accumulation in peripheral blood and infiltration of organs (i.e., lymph nodes, spleen, liver, kidney). As a result of bone marrow infiltration, one or all series are suppressed, generating pancytopenia (anemia, neutropenia and thrombocytopenia).Leukemia classification, based upon clinical and histogenetic criteria : Chronic lymphocytic (lymphoid) leukemia (liver). Tumor lymphocytic infiltrate into the portal tracts, which appear very enlarged, lacking normal structures. These tumor lymphoid cells resemble normal lymphocytes (small, monomorphic, round hyperchromatic homogenous nuclei, reduced cytoplasm), but are immature, monoclonal and non-functional. With evolution, the tumor cells will infiltrate the lobules. (H&E, ob. x10)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــChronic myeloid leukemia (liver)Leukemia is a monoclonal malignant proliferation of stem cells of bone marrow, with replacement of normal bone marrow by leukemic cells, accumulation in peripheral blood and infiltration of organs (i.e., lymph nodes, spleen, liver, kidney). As a result of bone marrow infiltration, one or all series are suppressed, generating pancytopenia (anemia, neutropenia and thrombocytopenia).Leukemia classification, based upon clinical and histogenetic criteria :
- Acute leukemias (proliferation of young, immature elements)
- Lymfoblastic
- Myeloblastic
Chronic leukemias (monoclonal proliferation of non-functional lymphoid and myeloid elements)
Lymphocytic (lymphoid)
Granulocytic (myeloid)
Chronic myeloid leukemia is a malignant lymphoid proliferation of all hematopoietic series, prominently granulocytic precursors. In 90 % of cases, t(9;22) is present (translocation between chromosomes 22 and 9). This results in formation of Philadelphia chromosome and BCR/ABL gene (which produces an abnormal protein with strong tyrosine-kinase activity). Chronic myeloid leukemia (liver). Pleomorphic tumor infiltrate : rare blast cells (myeloblasts, promyelocytes) and numerous myelocytes, neutrophils, basophils, eosinophils, metamyelocytes, mature leukocytes. These tumor cells infiltrate and dilate the portal tracts, but especially the sinusoids. (H&E, ob. x20) Chronic myeloid leukemia (liver). Pleomorphic tumor infiltrate : rare blast cells (myeloblasts, promyelocytes) and numerous myelocytes, neutrophils, basophils, eosinophils, metamyelocytes, mature leukocytes. These tumor cells infiltrate and dilate the portal tracts, but especially the sinusoids. (H&E, ob. x20) Chronic myeloid leukemia (liver). (H&E, ob. x40)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــHodgkin's lymphoma, Reed-Sternberg cellHodgkin's lymphoma is a primary malignant tumor of the lymph nodes, rarely affecting the extranodal lymphoid tissue. The diagnosis criteria are: tumor component (Reed-Sternberg cell - typical and variants) and a reactive component (normal mature lymphocytes, eosinophils, plasma cells, neutrophils, fibrosis and capillaries).Histological classification of Hodgkin's lymphoma (according to lymph node architecture, ratio between tumor and non-tumor components, morphology of Reed-Sternberg cell and compositon of reactive infiltrate) : Chronic myeloid leukemia (liver). (H&E, ob. x40)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــHodgkin's lymphoma, Reed-Sternberg cellHodgkin's lymphoma is a primary malignant tumor of the lymph nodes, rarely affecting the extranodal lymphoid tissue. The diagnosis criteria are: tumor component (Reed-Sternberg cell - typical and variants) and a reactive component (normal mature lymphocytes, eosinophils, plasma cells, neutrophils, fibrosis and capillaries).Histological classification of Hodgkin's lymphoma (according to lymph node architecture, ratio between tumor and non-tumor components, morphology of Reed-Sternberg cell and compositon of reactive infiltrate) :[list=roman_mare] [*] (Non-classical) Nodular lymphocyte predominant Hodgkin's lymphoma (5 %)[*] Classical Hodgkin's lymphoma[list=a_mic] [*] Nodular sclerosing (60 - 80 %)[*] Lymphocyte-rich (5 %)[*] Mixed cellularity (15 - 30 %)[*] Lymphocyte depleted (< 1 %)[/list] [/list] Variants of Reed-Sternberg cell (RSC) :
- Hodgkin's cell (atypical mononuclear RSC)
- Lacunar Reed-Sternberg cell (RSC)
- Pleomorphic Reed-Sternberg cell (RSC)
- Limfo-histiocytic ("pop-corn") variant
- "Mummy" Reed-Sternberg cell (RSC)
 Presence of typical Reed-Sternberg cell and reactive component are mandatory for diagnosis of Hodgkin's lymphoma. Characteristics of typical Reed-Sternberg cell : size between 20 - 50 microns; abundant, amphofilic, finely granular/homogenous cytoplasm; two mirror-image nuclei ("owl eyes") each with an eosinophilic nucleolus and a thick nuclear membrane (chromatin is distributed on the inner surface of the nuclear membrane, generating a halo image around the nucleolus). Reed-Sternberg cell has a B-cell origin. (H&E, ob.x40)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــReed-Sternberg cellHodgkin's lymphoma is a primary malignant tumor of the lymph nodes, rarely affecting the extranodal lymphoid tissue. The diagnosis criteria are : tumor component (Reed-Sternberg cell - typical and variants) and a reactive component (normal mature lymphocytes, eosinophils, plasma cells, neutrophils, fibrosis and capillaries).Histological classification of Hodgkin's lymphoma (according to lymph node architecture, ratio between tumor and non-tumor components, morphology of Reed-Sternberg cell and compositon of reactive infiltrate) : Presence of typical Reed-Sternberg cell and reactive component are mandatory for diagnosis of Hodgkin's lymphoma. Characteristics of typical Reed-Sternberg cell : size between 20 - 50 microns; abundant, amphofilic, finely granular/homogenous cytoplasm; two mirror-image nuclei ("owl eyes") each with an eosinophilic nucleolus and a thick nuclear membrane (chromatin is distributed on the inner surface of the nuclear membrane, generating a halo image around the nucleolus). Reed-Sternberg cell has a B-cell origin. (H&E, ob.x40)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــReed-Sternberg cellHodgkin's lymphoma is a primary malignant tumor of the lymph nodes, rarely affecting the extranodal lymphoid tissue. The diagnosis criteria are : tumor component (Reed-Sternberg cell - typical and variants) and a reactive component (normal mature lymphocytes, eosinophils, plasma cells, neutrophils, fibrosis and capillaries).Histological classification of Hodgkin's lymphoma (according to lymph node architecture, ratio between tumor and non-tumor components, morphology of Reed-Sternberg cell and compositon of reactive infiltrate) :[list=roman_mare] [*] (Non-classical) Nodular lymphocyte predominant Hodgkin's lymphoma (5 %)[*] Classical Hodgkin's lymphoma[list=a_mic] [*] Nodular sclerosing (60 - 80 %)[*] Lymphocyte-rich (5 %)[*] Mixed cellularity (15 - 30 %)[*] Lymphocyte depleted (< 1 %)[/list] [/list] Variants of Reed-Sternberg cell (RSC) :
- Hodgkin's cell (atypical mononuclear Reed-Sternberg cell (RSC)
- Lacunar Reed-Sternberg cell (RSC)
- Pleomorphic Reed-Sternberg cell (RSC)
- Limfo-histiocytic ("pop-corn") variant
- "Mummy" Reed-Sternberg cell (RSC)
 Hodgkin's lymphoma (H&E, ob.x20) Hodgkin's lymphoma (H&E, ob.x20)
Typical Reed-Sternberg cell : size between 20 - 50 microns; abundant, amphofilic, finely granular/homogenous cytoplasm; two mirror-image nuclei ("owl eyes") each with an eosinophilic nucleolus and a thick nuclear membrane (chromatin is distributed on the inner surface of the nuclear membrane, generating a halo image around the nucleolus).
Sternberg-Reed cell (II) Hodgkin's lymphoma. Variants of Reed-Sternberg cell (H&E, ob.x20) : Hodgkin's lymphoma. Variants of Reed-Sternberg cell (H&E, ob.x20) :
- Hodgkin's cell (atypical mononuclear Reed-Sternberg cell is a variant of Reed-Sternberg cell, which has the same characteristics, but is mononucleated
- Lacunar Reed-Sternberg cell is large, with a single hyperlobated nucleus, multiple, small nucleoli and eosinophilic cytoplasm which is retracted around the nucleus, creating an empty space ("lacunae")
- Pleomorphic Reed-Sternberg cell has multiple irregular nuclei
- "Pop-corn" Reed-Sternberg cell (lympho-histiocytic variant) is a small cell, with a very lobulated nucleus, small nucleoli.
- "Mummy" Reed-Sternberg cell has a compact nucleus, no nucleolus and basophilic cytoplasm
ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــDiffuse lymphocytic non-Hodgkin's lymphomaNon-Hodgkin's malignant lymphomas comprise a heterogeneous group of malignancies of the immune system (except Hodgkin's lymphoma). The majority (85%) results from a proliferation of B-cells; only 15 % derives from T/NK cells. Non-Hodgkin's malignant lymphomas comprise a heterogeneous group of malignancies of the immune system (except Hodgkin's lymphoma). The majority (85%) results from a proliferation of B-cells; only 15 % derives from T/NK cells. Non-Hodgkin's malignant lymphomas comprise a heterogeneous group of malignancies of the immune system (except Hodgkin's lymphoma). The majority (85%) results from a proliferation of B-cells; only 15 % derives from T/NK cells. |
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:12 am الإثنين 19 نوفمبر 2018, 12:12 am | |
| Pathology Slides : Breast pathology
اضغط على الصورة للتكبير -ـ Click on image to enlarge size
Fibroadenoma is the most common benign tumor of the female breast. Breast carcinoma is the second cause of cancer death in females in the world. Both seem to arise on a hyperestrogenism status.
.................................................................................
Fibroadenoma of the breast
Fibroadenoma of the breast is a benign tumor composed of two elements : epithelium and stroma. It is nodular and encapsulated, included in breast. The epithelial proliferation appears in a single terminal ductal unit and describes duct-like spaces surrounded by a fibroblastic stroma. Depending on the proportion and the relationship between these two components, there are two main histological features : intracanalicular and pericanalicular. Often, both types are found in the same tumor. Intracanalicular fibroadenoma (photo A) : stromal proliferation predominates and compresses the ducts, which are irregular, reduced to slits. Pericanalicular fibroadenoma (photo B) : fibrous stroma proliferates around the ductal spaces, so that they remain round or oval, on cross section. The basement membrane is intact. (H&E, ob. x10)


ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Invasive ductal carcinoma of the breast

Invasive (infiltrating) ductal carcinoma of the breast is a malignant epithelial tumor resulted from proliferation of ductal epithelium of breast. It is the most common type of breast cancer (70 - 80 %). Atypical tumor cells form ribbons, tubules or nests, broke the basement membrane of the duct and infiltrate the surrounding tissues (fat tissue - photo, skeletal muscle and/or skin). Tumor cells induce desmoplastic reaction in stroma (abundant fibrosis, collagen). (H&E, ob. x20)
|
|   | | ابراهيم الشنطي
Admin

عدد المساهمات : 75802
تاريخ التسجيل : 28/01/2013
العمر : 78
الموقع : الاردن
 |  موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides موضوع: رد: مكتبة الصور الطبية : - باثولوجى -- Pathology slides  الإثنين 19 نوفمبر 2018, 12:12 am الإثنين 19 نوفمبر 2018, 12:12 am | |
| Pathology Slides : Female Genital System Pathology اضغط على الصورة للتكبير -ـ Click on image to enlarge sizeMain entities of the female genital system pathology :
- in vagina : benign epithelial tumors (papilloma or condilloma acuminate)
- in cervix uteri : inflammatory lesions (chronic cervicitis), dysplasia (CIN grades I, II or III) and malignant tumors (squamous cell carcinoma).
- in corpus uteri : endometritis, endometrial hyperplasia, benign epithelial (endometrial polyp) and conjunctive (leiomyoma) tumors, and malignant tumors (endometrial carcinoma).
- in fallopian tubes : inflammatory lesions (acute and chronic salpingitis)
- in ovary : cysts and ovarian tumors.
The most frequent diseases of pregnancy are : ectopic pregnancy, abortion, trophoblastic (placental) tumors (hydatiform mole, invasive mole and gestational choriocarcinoma)........................................................................Simple typical hyperplasia of endometriumEndometrial hyperplasia (hyperplasia of endometrium) is a dishormonal lesion, produced by hyperestrinism, which generates the glandular and stromal proliferation of endometrium. It may be simple or complex, typical or atypical. Endometrial hyperplasia may regress or may transform into adenocarcinoma. Simple, typical hyperplasia has a low risk of malignancy (less than 1 %), while the risk for complex, atypical hyperplasia is about 25 %. Simple, typical hyperplasia of endometrium. The hyperplastic endometrium consists in proliferated epithelium with quasi-normal appearing (stratified, tall columnar, or cuboidal) and proliferated cells in stroma. Often, the glands are dilated (cystic "Swiss cheese" hyperplasia). (H&E, ob. x10) Simple, typical hyperplasia of endometrium. The hyperplastic endometrium consists in proliferated epithelium with quasi-normal appearing (stratified, tall columnar, or cuboidal) and proliferated cells in stroma. Often, the glands are dilated (cystic "Swiss cheese" hyperplasia). (H&E, ob. x10)
Simple typical hyperplasia of endometrium (detail) 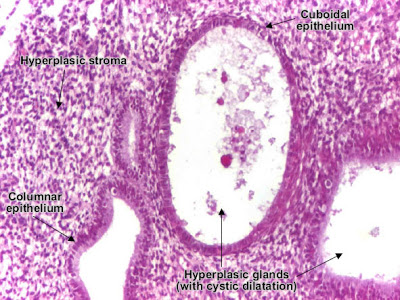 Simple, typical hyperplasia of endometrium. (H&E, ob. x20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــEndometrioid carcinoma of endometriumEndometrioid adenocarcinoma of the endometrium is a malignant epithelial tumor. It appears on a background of endometrial hyperplasia, in hyperestrogenism. Tumor cells are atypical and form irregular glands, with multiple lumens, stratification. The stroma is reduced, producing the "back to back" aspect of the tumor glands. The myometrium is not infiltrated. (H&E, ob. x10) Simple, typical hyperplasia of endometrium. (H&E, ob. x20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــEndometrioid carcinoma of endometriumEndometrioid adenocarcinoma of the endometrium is a malignant epithelial tumor. It appears on a background of endometrial hyperplasia, in hyperestrogenism. Tumor cells are atypical and form irregular glands, with multiple lumens, stratification. The stroma is reduced, producing the "back to back" aspect of the tumor glands. The myometrium is not infiltrated. (H&E, ob. x10)
Endometrioid carcinoma of endometrium (detail) Endometrioid adenocarcinoma of the endometrium. (H&E, ob. x20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــUterine curettage biopsyPlacenta has two important components : chorionic villi and decidua. The purpose of an uterine curettage biopsy might be therapeutic or abortive.Chorionic villi Endometrioid adenocarcinoma of the endometrium. (H&E, ob. x20)ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــUterine curettage biopsyPlacenta has two important components : chorionic villi and decidua. The purpose of an uterine curettage biopsy might be therapeutic or abortive.Chorionic villi  Placenta (chorionic plate) villi - fetal component of placenta has a central core (vessels and mesenchymal cells) covered by trophoblast (cytotrophoblast and sycytiotrophoblast). (H&E, ob. x10) Placenta (chorionic plate) villi - fetal component of placenta has a central core (vessels and mesenchymal cells) covered by trophoblast (cytotrophoblast and sycytiotrophoblast). (H&E, ob. x10)
Decidua Placenta (basal plate) decidua - maternal component of placenta : large decidual cells, with central nucleus, eosinophilic cytoplasm, well delineated. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــLeiomyoma (uterus) Placenta (basal plate) decidua - maternal component of placenta : large decidual cells, with central nucleus, eosinophilic cytoplasm, well delineated. (H&E, ob. x20)ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــLeiomyoma (uterus) Uterine leiomyoma is a benign connective tissue tumor of the smooth muscle cells of the myometrium. Tumor cells resemble normal cells (uniform, elongated, spindle-shaped, with a cigar-shaped nucleus) and form bundles with different directions (whirled). The tumor may present areas of fibrosis, calcification and/or hemorrhage. The tumor is well circumscribed, but not encapsulated. (Hematoxylin-eosin, ob. x10) Uterine leiomyoma is a benign connective tissue tumor of the smooth muscle cells of the myometrium. Tumor cells resemble normal cells (uniform, elongated, spindle-shaped, with a cigar-shaped nucleus) and form bundles with different directions (whirled). The tumor may present areas of fibrosis, calcification and/or hemorrhage. The tumor is well circumscribed, but not encapsulated. (Hematoxylin-eosin, ob. x10) |
|   | | | | مكتبة الصور الطبية : - باثولوجى -- Pathology slides |  |
|
مواضيع مماثلة |  |
|
| | صلاحيات هذا المنتدى: | لاتستطيع الرد على المواضيع في هذا المنتدى
| |
| |
| |
